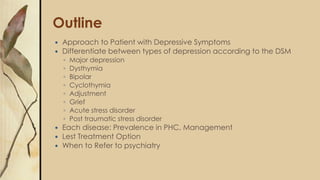
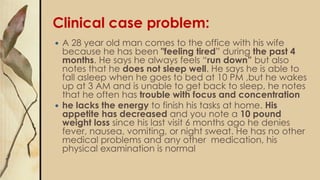
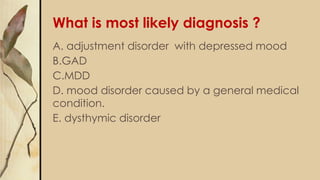
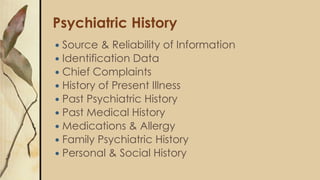
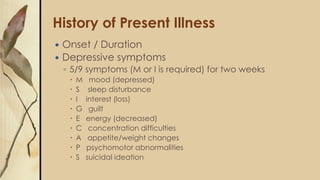
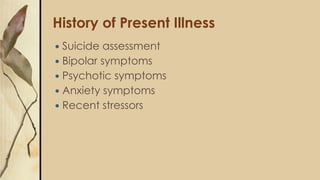
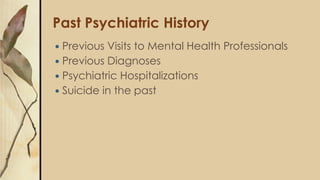
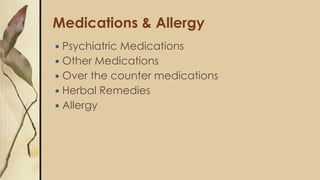
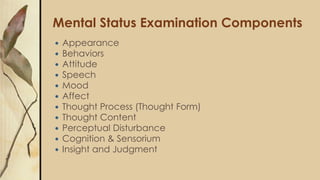
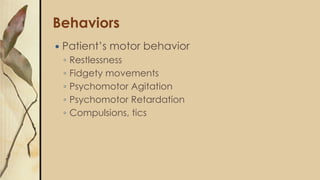
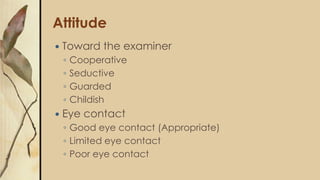
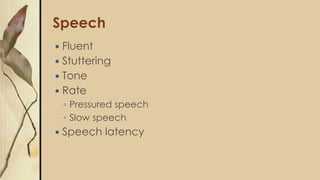
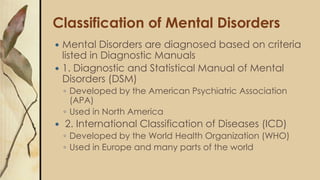
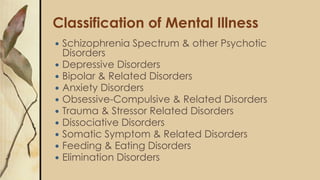
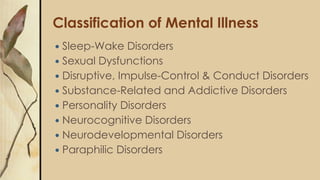
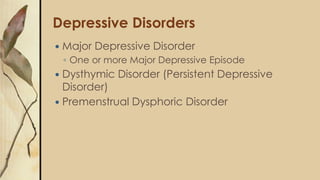
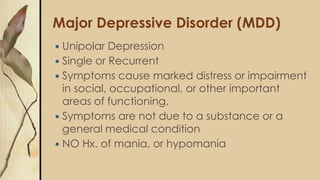
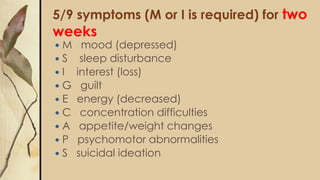
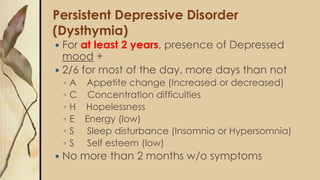
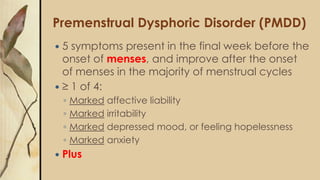
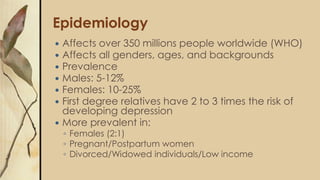
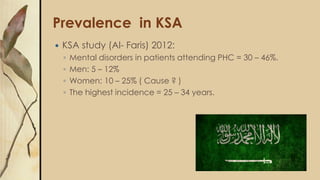
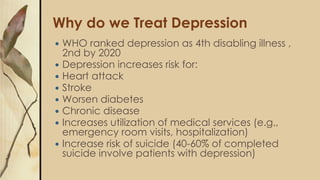
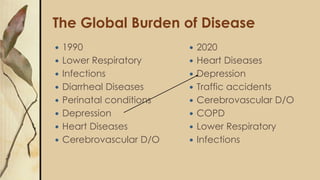
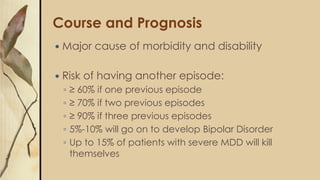
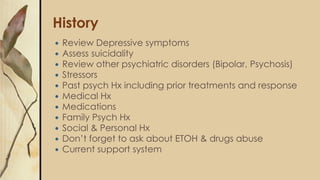
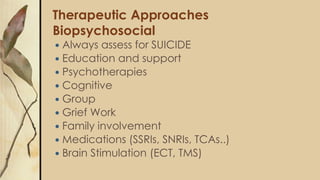
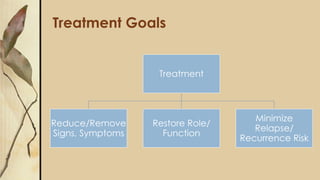
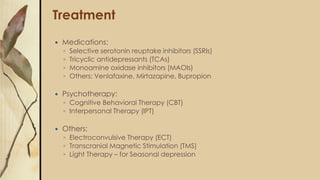
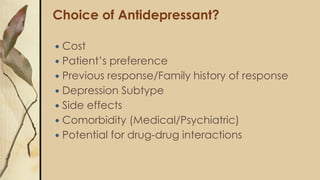
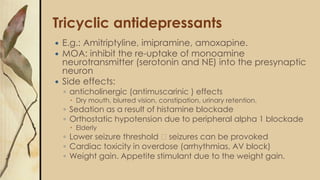
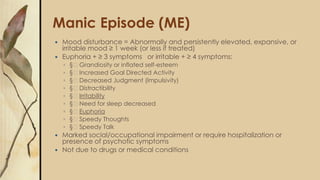
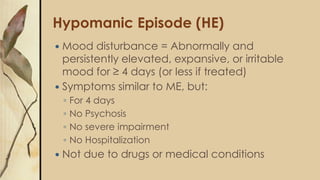
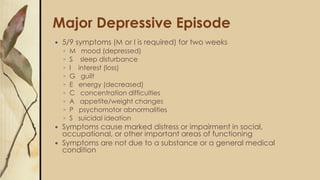
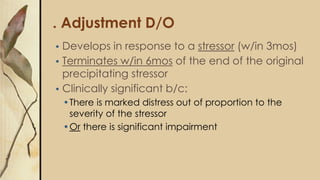
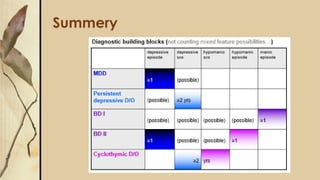
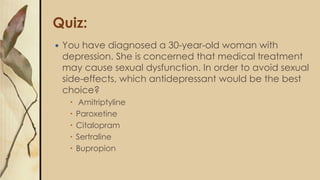
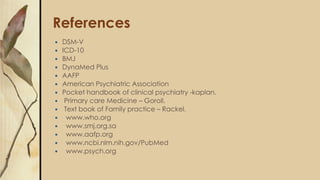
This document provides an outline for a presentation on depressive disorders. It begins with approaching patients with depressive symptoms and differentiating between types of depression according to the DSM. The most common types are described along with their prevalence, management, and treatment options. Guidelines are provided for when to refer patients to psychiatry. A clinical case example is presented and the most likely diagnosis is discussed. The document also covers interviewing psychiatric patients in primary health care and includes sections on goal of assessment, components of history and mental status examination.