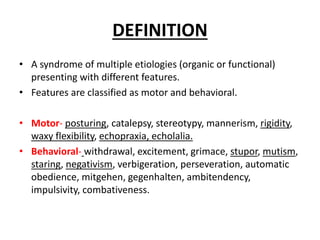
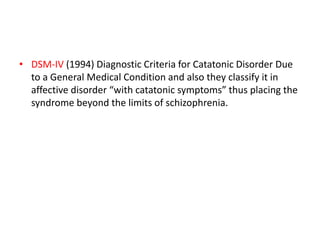
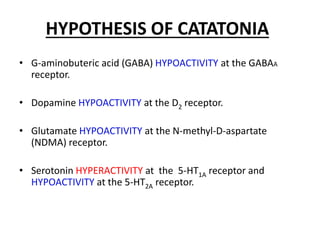
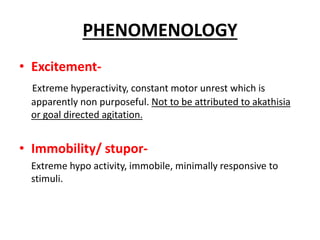
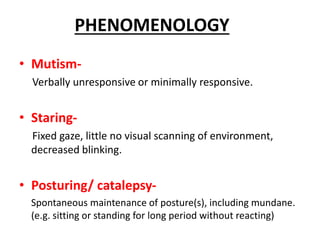
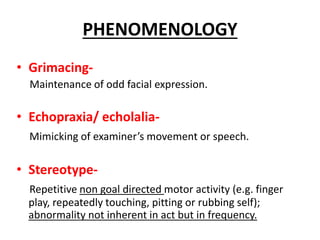
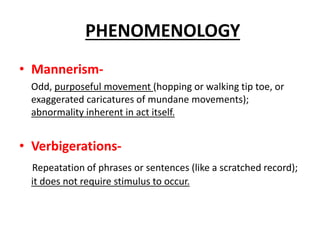
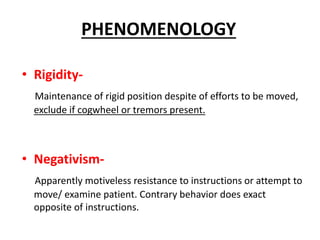
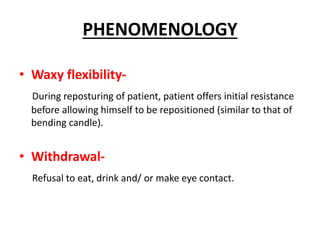
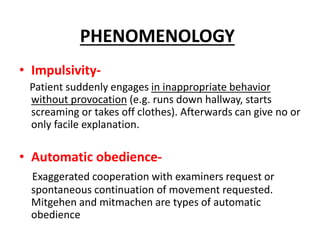
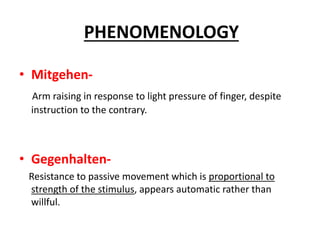
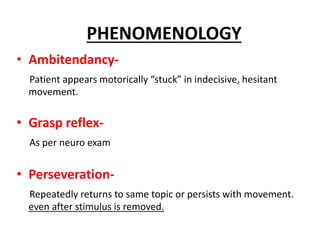
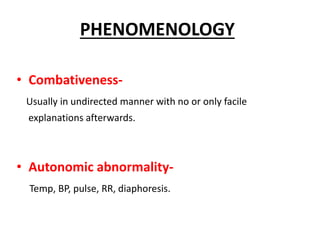
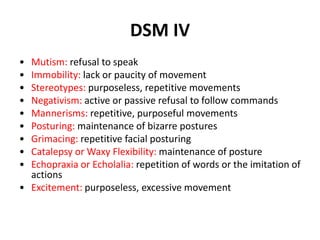
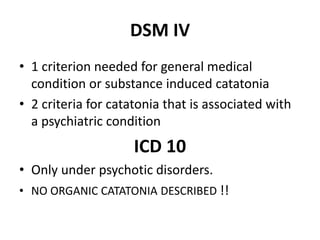
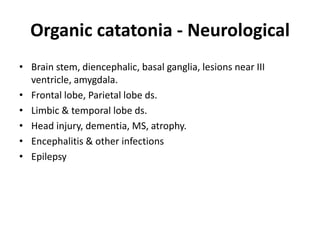
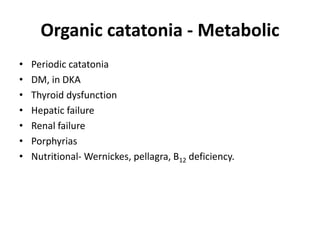
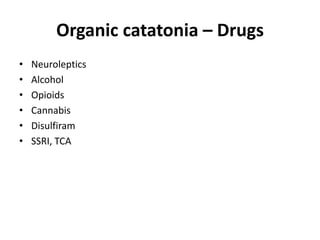
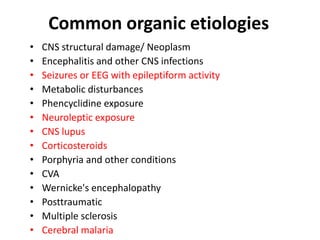
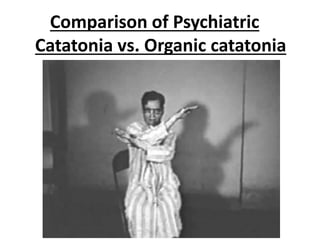
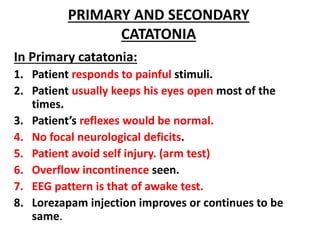
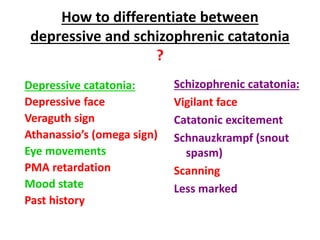
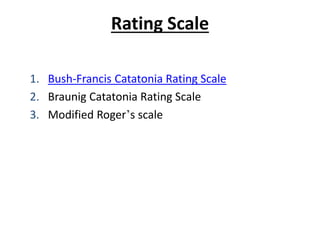
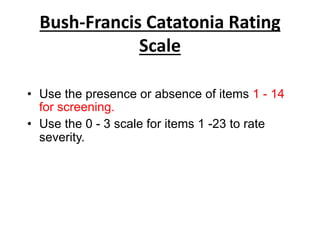
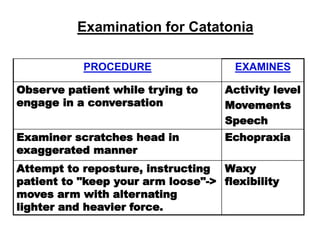
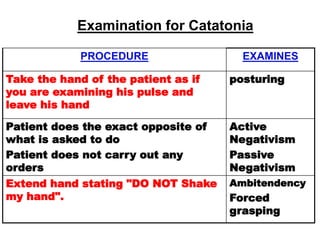
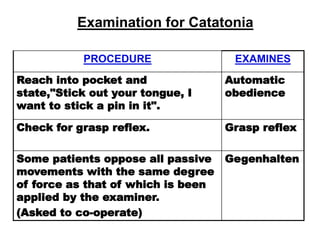
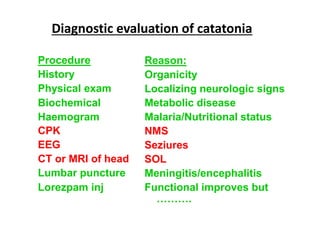
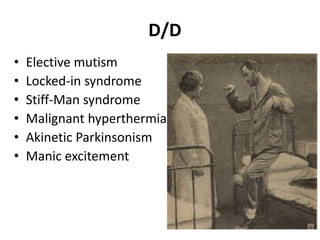
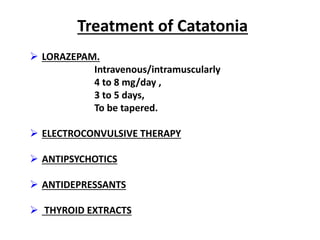
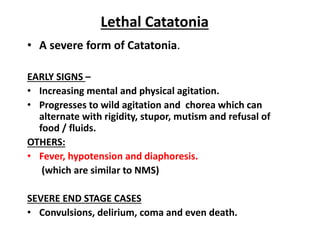
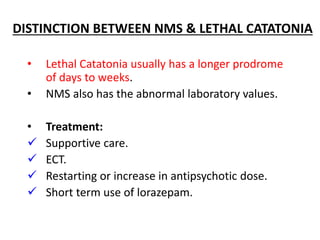
The document provides an overview of catatonia, a syndrome characterized by various motor and behavioral symptoms, with historical context and hypotheses regarding its causes, including neurological and psychological factors. It details distinguishing features, diagnostic criteria from DSM-IV and ICD-10, and compares psychiatric versus organic catatonia. Treatment options include lorazepam, electroconvulsive therapy, antipsychotics, and antidepressants, emphasizing the importance of addressing both primary and secondary causes.