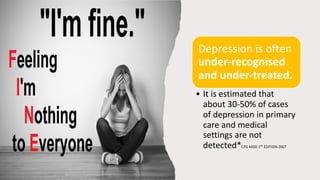
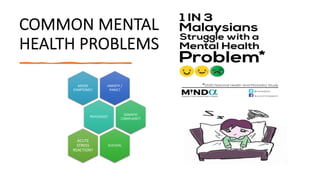
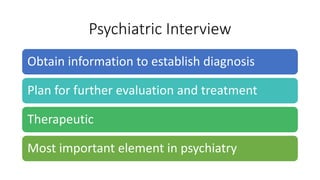
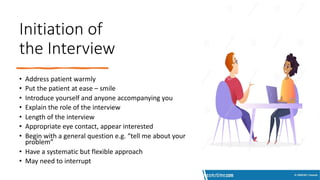
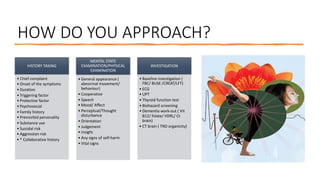
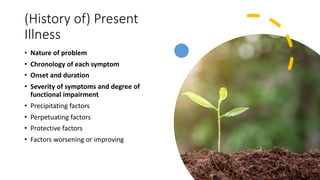
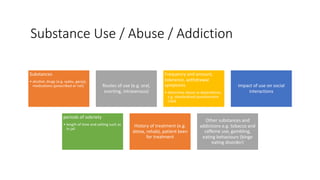
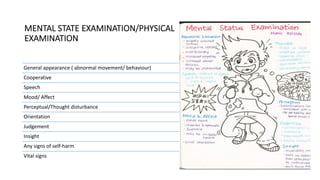
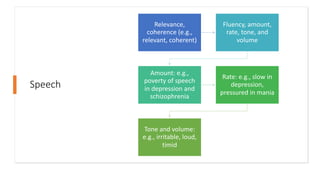
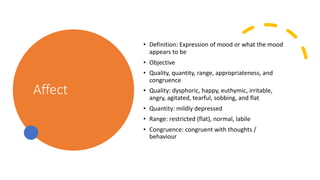
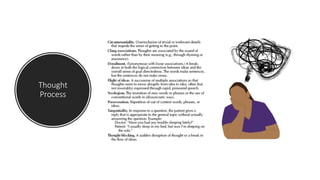
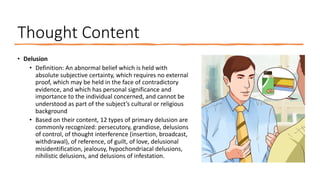
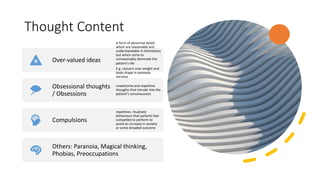
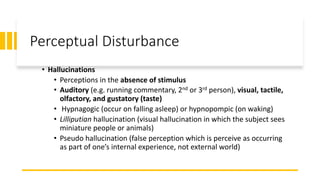
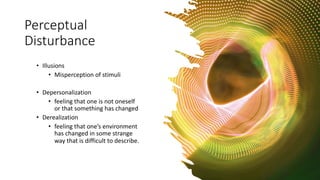
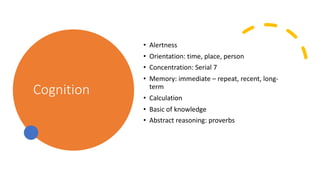
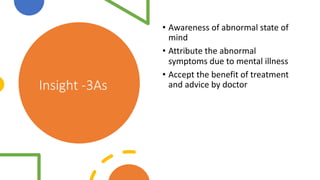
This document provides guidance on conducting basic psychiatric history taking and mental state examinations. It outlines key areas to assess including chief complaints, psychiatric history, substance use, medical history, family history, development, and social factors. The mental state examination should evaluate appearance, speech, mood, affect, thought processes, thought content, perceptual disturbances, cognition, insight, and judgment. Depression is common but often underrecognized in primary care settings. Thorough evaluation following these areas can help detect psychiatric illnesses early and improve patient outcomes.