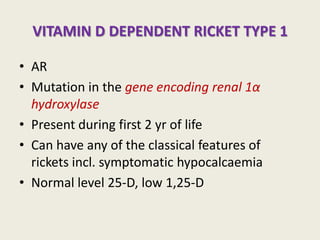
1) Vitamin D deficiency can cause rickets, a softening and weakening of bones in children. It is most common in infants and children with inadequate vitamin D intake or sunlight exposure.
2) Symptoms of rickets include bowed legs, soft skull, and delayed growth. Diagnosis is confirmed by x-rays showing widened growth plates and undermineralized bones.
3) Treatment involves high dose vitamin D supplements to raise vitamin D levels, along with ensuring adequate calcium and phosphate intake. Daily vitamin D supplements can help prevent deficiency.