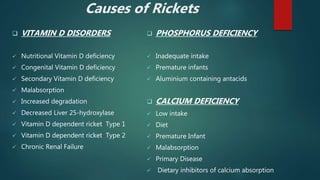
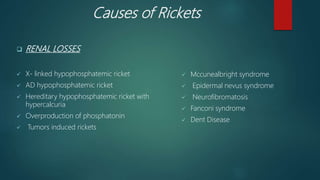
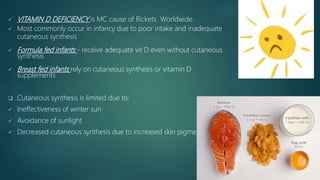
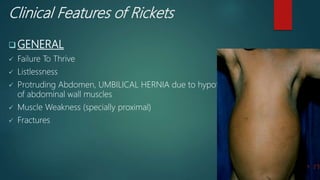
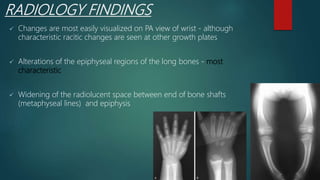
Rickets is a disease of growing bones caused by inadequate mineralization due to vitamin D deficiency or disorders of calcium and phosphorus. It occurs in children before bone growth plate fusion. Common causes include nutritional deficiencies of vitamin D, calcium, or phosphorus. Clinical features include bone softening and deformities, muscle weakness, and hypocalcemic symptoms. Diagnosis is confirmed by blood tests and radiographic findings of widened growth plates. Treatment involves high dose vitamin D supplementation along with adequate calcium and phosphorus intake.