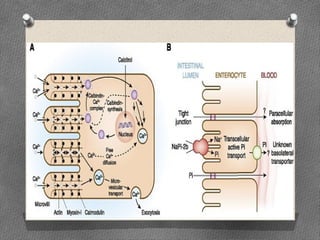
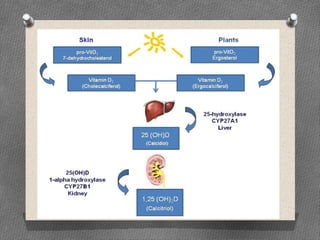
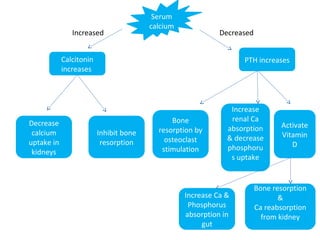
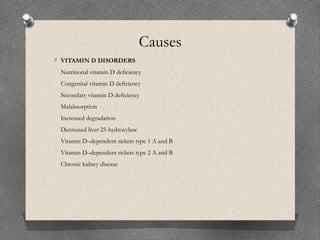
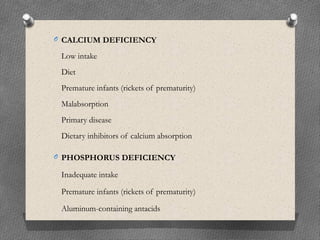
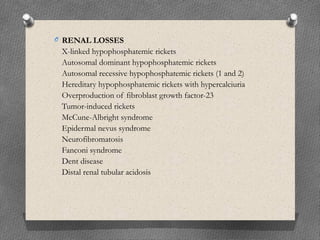
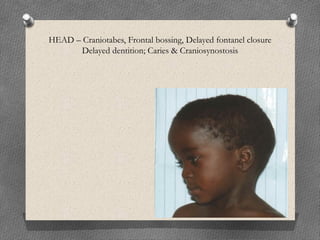
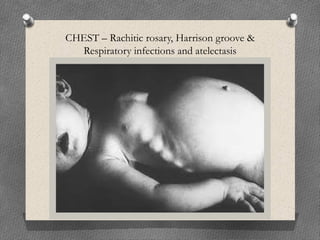
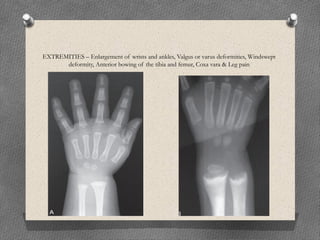
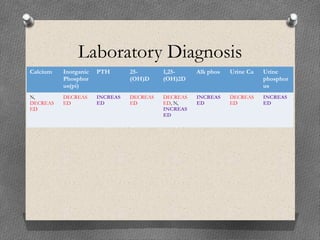
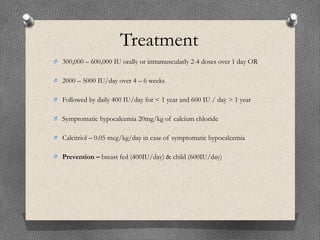
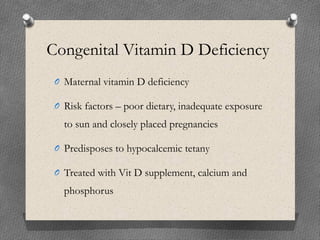
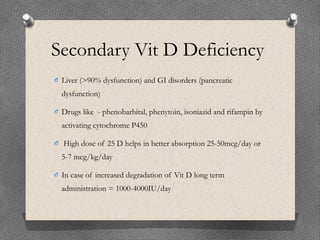
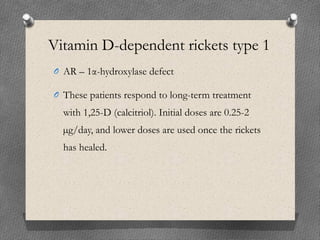
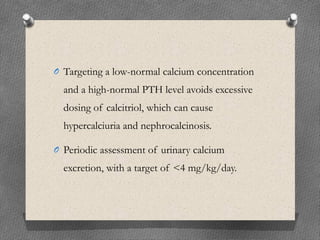
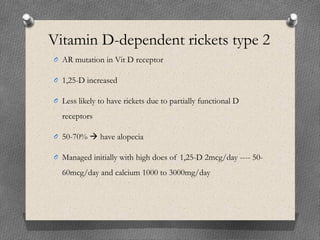
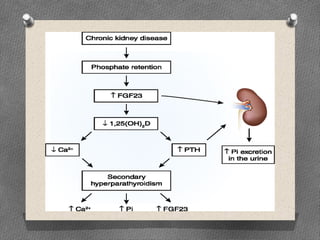
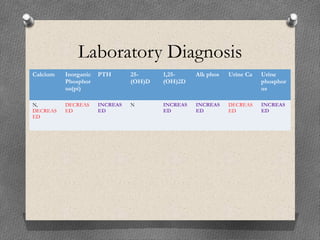
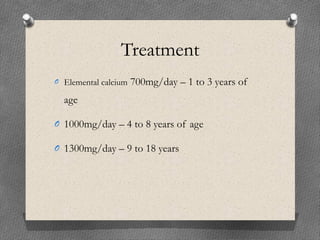
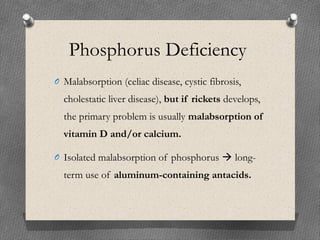
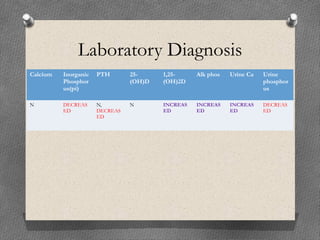
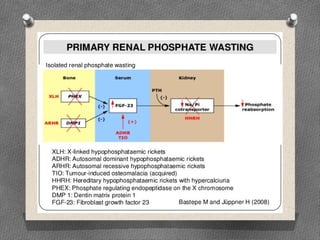
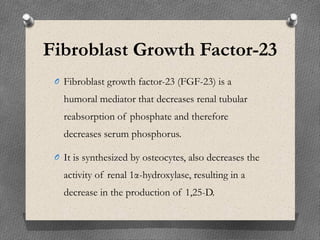
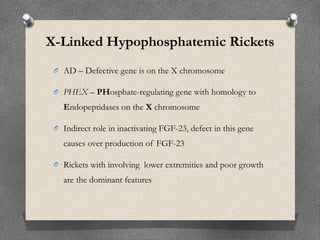
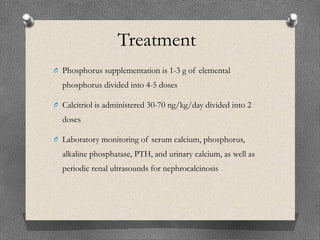
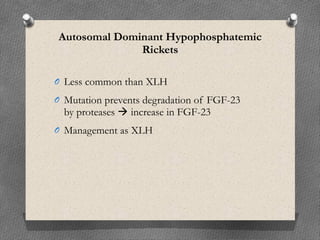
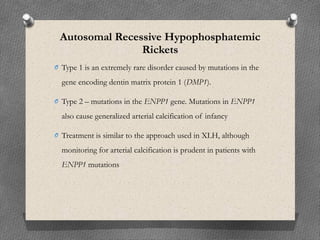
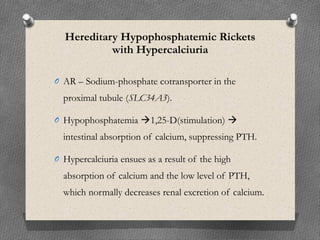
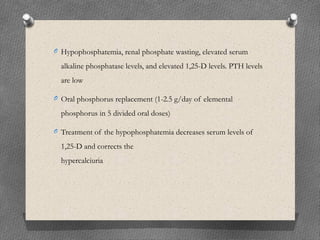
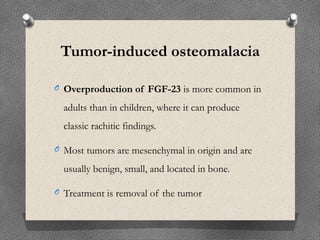
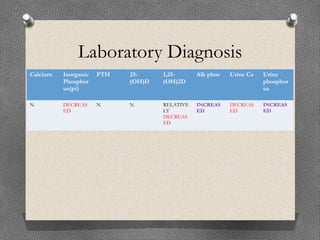
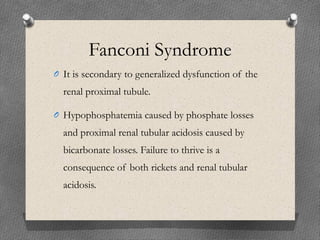
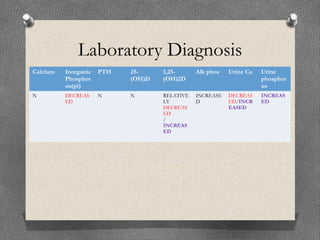
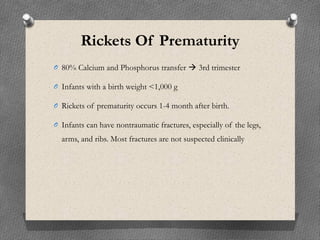
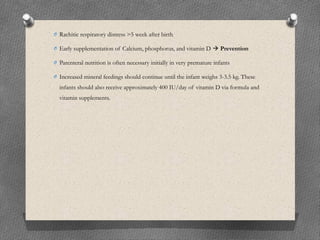
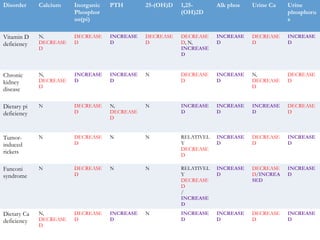
This document summarizes calcium homeostasis and rickets. It discusses how parathyroid hormone (PTH), calcitonin, vitamin D, and other factors regulate calcium levels in the blood and bone. It also describes the causes, signs, symptoms, and treatments of rickets, which is a softening and weakening of bones in children due to vitamin D deficiency or other nutritional deficiencies that limit bone mineralization. The treatment for different types of rickets depends on the underlying cause but may involve calcium, vitamin D, phosphorus supplementation, or drugs like calcitriol. Laboratory tests can help diagnose rickets based on levels of calcium, phosphorus, PTH, vitamin D metabolites and other markers.