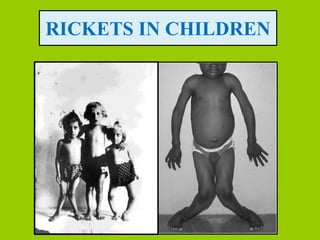
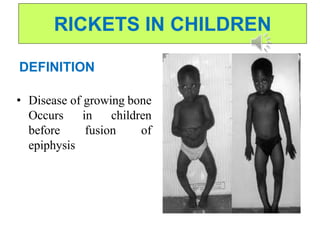
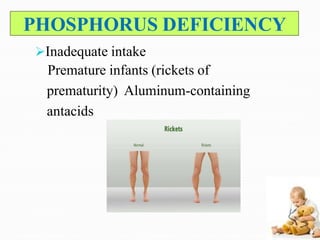
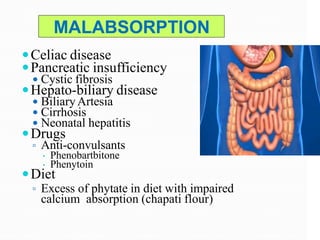
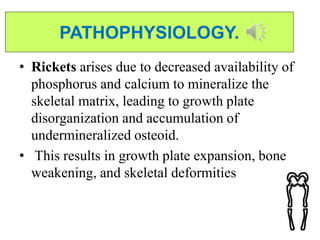
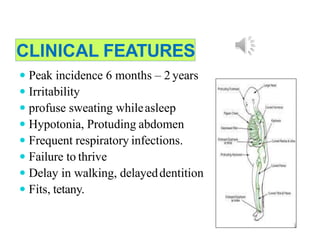
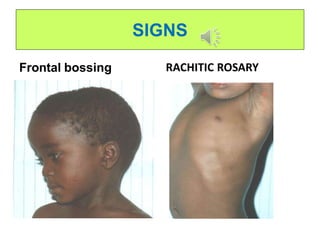
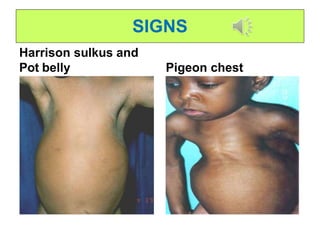
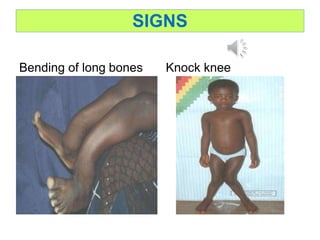
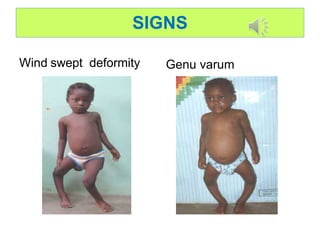
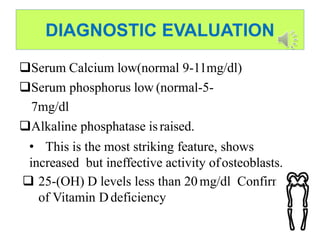
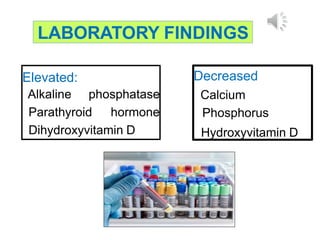
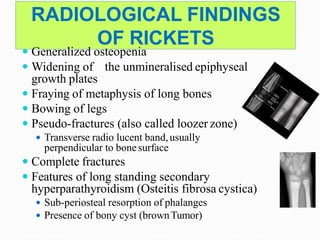
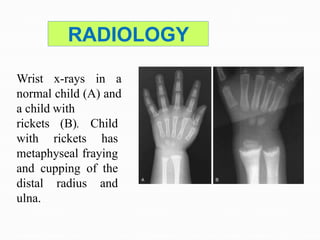
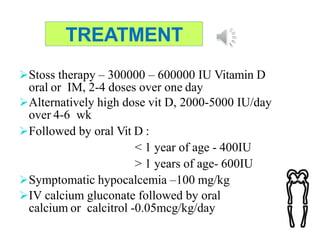
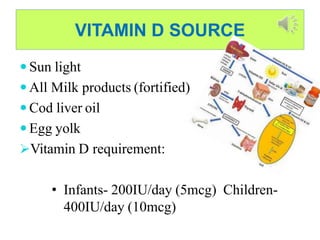
This document discusses rickets in children. Rickets is a disease of growing bones caused by vitamin D deficiency and/or lack of calcium and phosphorus. It commonly affects infants and young children before bone growth plates have closed. The main causes are nutritional vitamin D deficiency from lack of sunlight exposure or vitamin D-fortified foods, malabsorption issues that prevent calcium absorption, and rare genetic disorders. Clinical features include bone pain, soft bones that can fracture or deform, and bowed legs. Diagnosis involves blood tests showing low calcium and phosphorus and high alkaline phosphatase levels. Treatment focuses on high dose vitamin D supplementation and ensuring adequate calcium intake to mineralize bones.