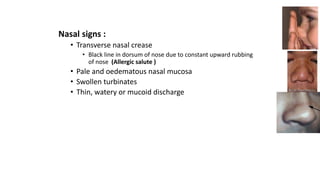
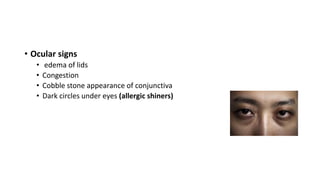
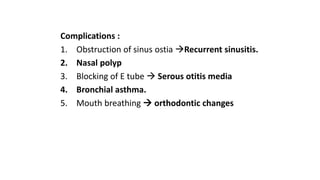
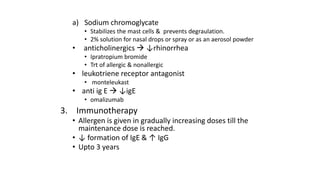
This document summarizes allergic rhinitis, including its causes, pathogenesis, symptoms, signs, diagnosis, complications, and treatment. Allergic rhinitis is an IgE-mediated immunologic response in the nasal mucosa to airborne allergens. It can be seasonal or perennial depending on the allergen. Symptoms include sneezing, nasal obstruction, rhinorrhea, and itching. Diagnosis involves history, examination showing signs like nasal crease or edema, and tests like skin tests or RAST. Complications include sinusitis, nasal polyps, or asthma. Treatment options include avoidance of allergens, antihistamines, decongestants, corticosteroids,