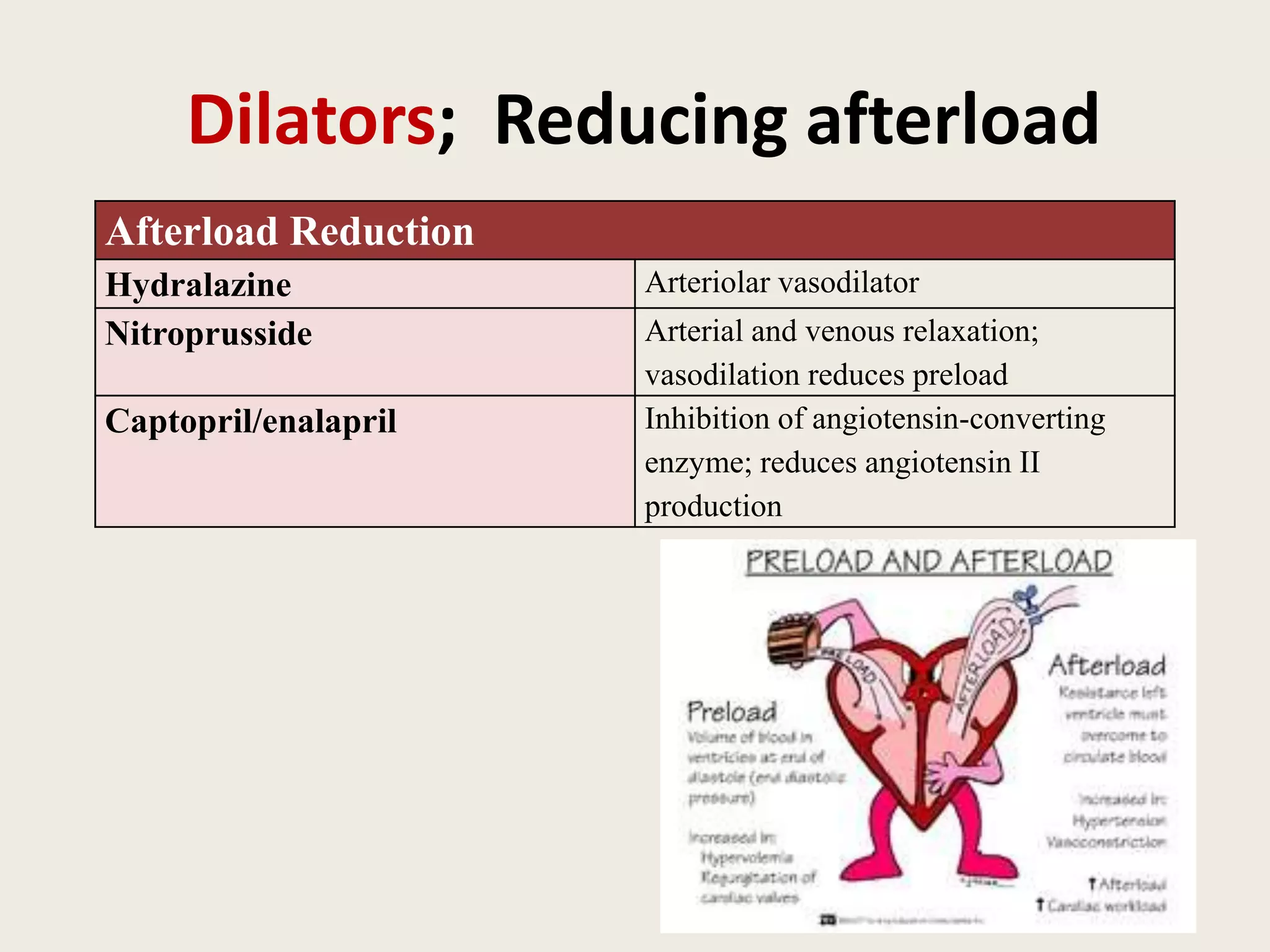
This document discusses congestive heart failure in children. It defines CHF as the heart's inability to meet metabolic demands due to reduced cardiac output or inability to dispose of venous return. Key factors affecting cardiac performance are preload, afterload, and contractility. Compensatory mechanisms in heart failure involve cardiac, systemic, and neurohormonal responses. Etiologies of pediatric CHF include congenital heart defects, cardiomyopathies, and acquired conditions. The document outlines approaches to diagnosis, treatment including medications to reduce preload and afterload, and non-pharmacological options.