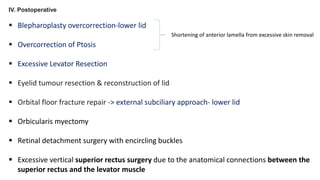
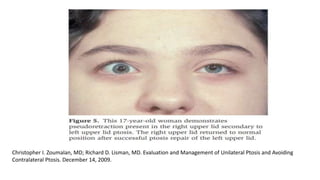
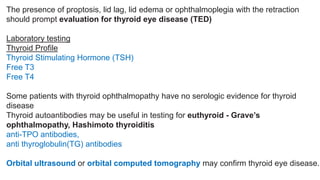
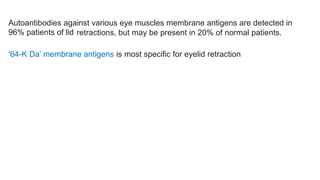
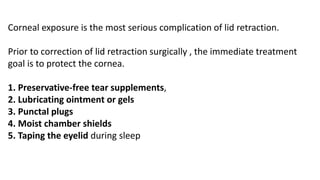
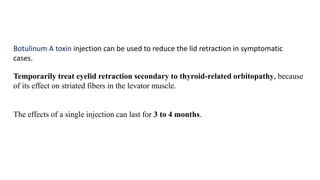
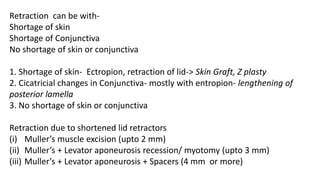
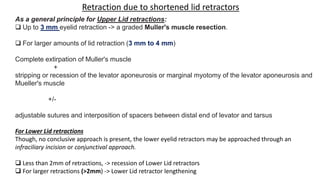
The symposium presented by Dr. Tanvi Gupta focused on lid retraction, including its etiopathology caused by factors such as levator muscle overactivity, sympathetic hyperactivity, and various conditions like thyroid eye disease. The document detailed different causes of lid retraction, including inflammatory, congenital, mechanical, and traumatic origins, as well as treatment approaches like surgical interventions and botulinum toxin injections. Management strategies and diagnostic evaluations for conditions leading to eyelid retractions were also highlighted.