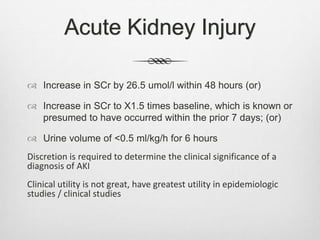
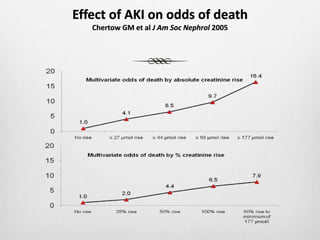
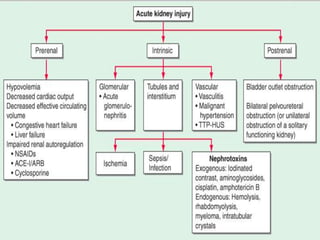
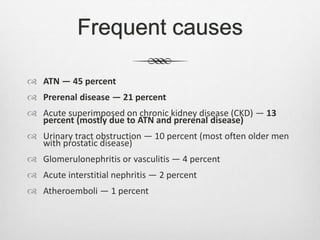
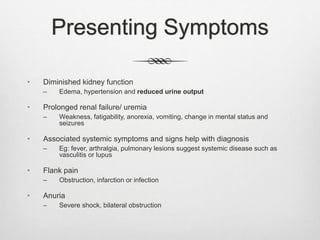
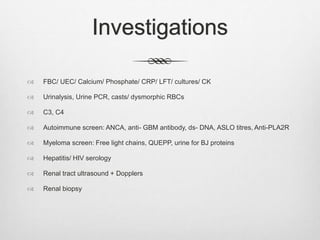
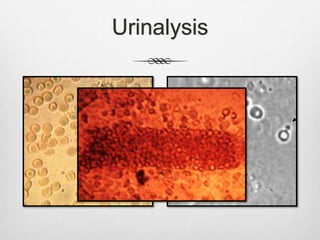
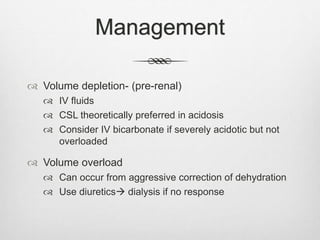
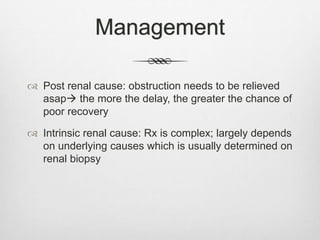
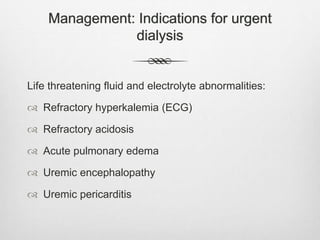
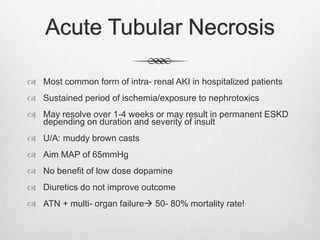
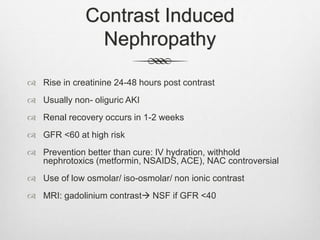
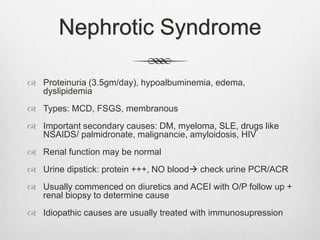
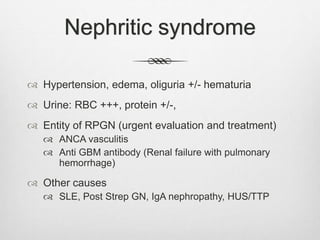
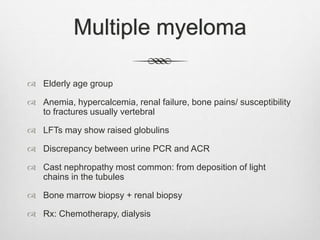
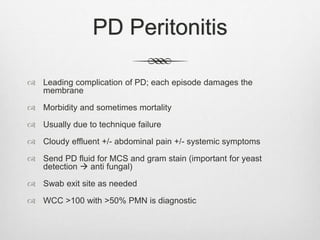
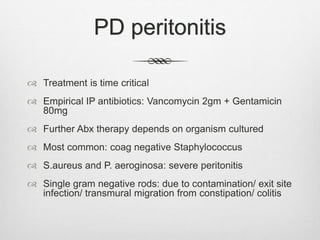
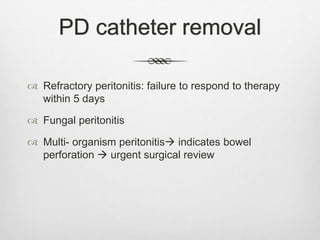
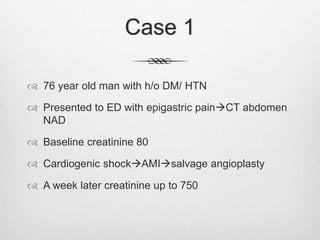
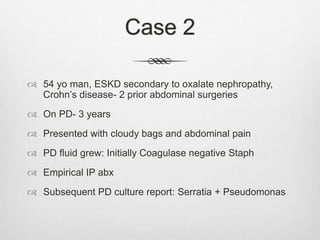
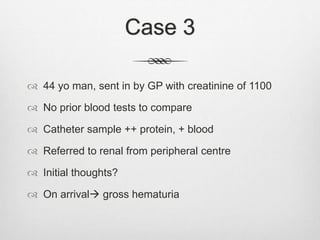
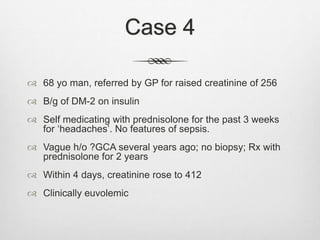
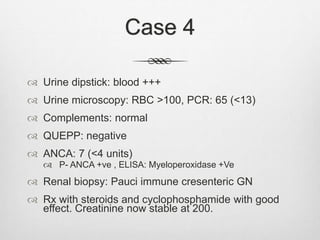
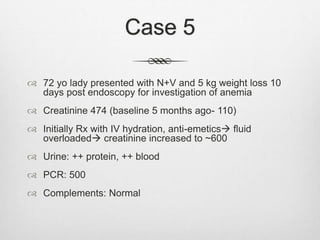
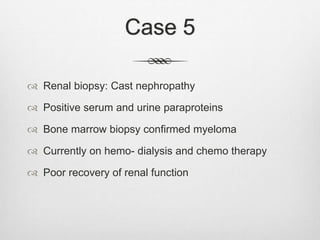
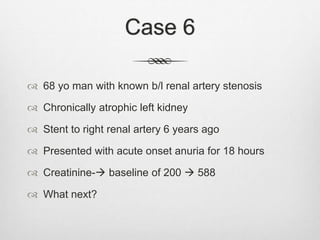
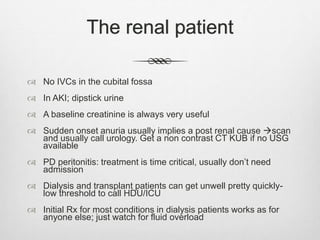
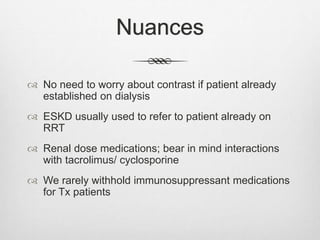
This document provides an overview of acute kidney injury (AKI), including definitions, causes, presentations, investigations, and management. It discusses the most common causes of AKI as being acute tubular necrosis, prerenal disease, and acute injury superimposed on chronic kidney disease. It also reviews peritoneal dialysis peritonitis and includes summaries of 6 case examples involving AKI, peritonitis, myeloma, vasculitis, and renal artery stenosis. Key points for managing renal patients are highlighted such as the importance of a baseline creatinine and treating peritonitis in a time-critical manner.