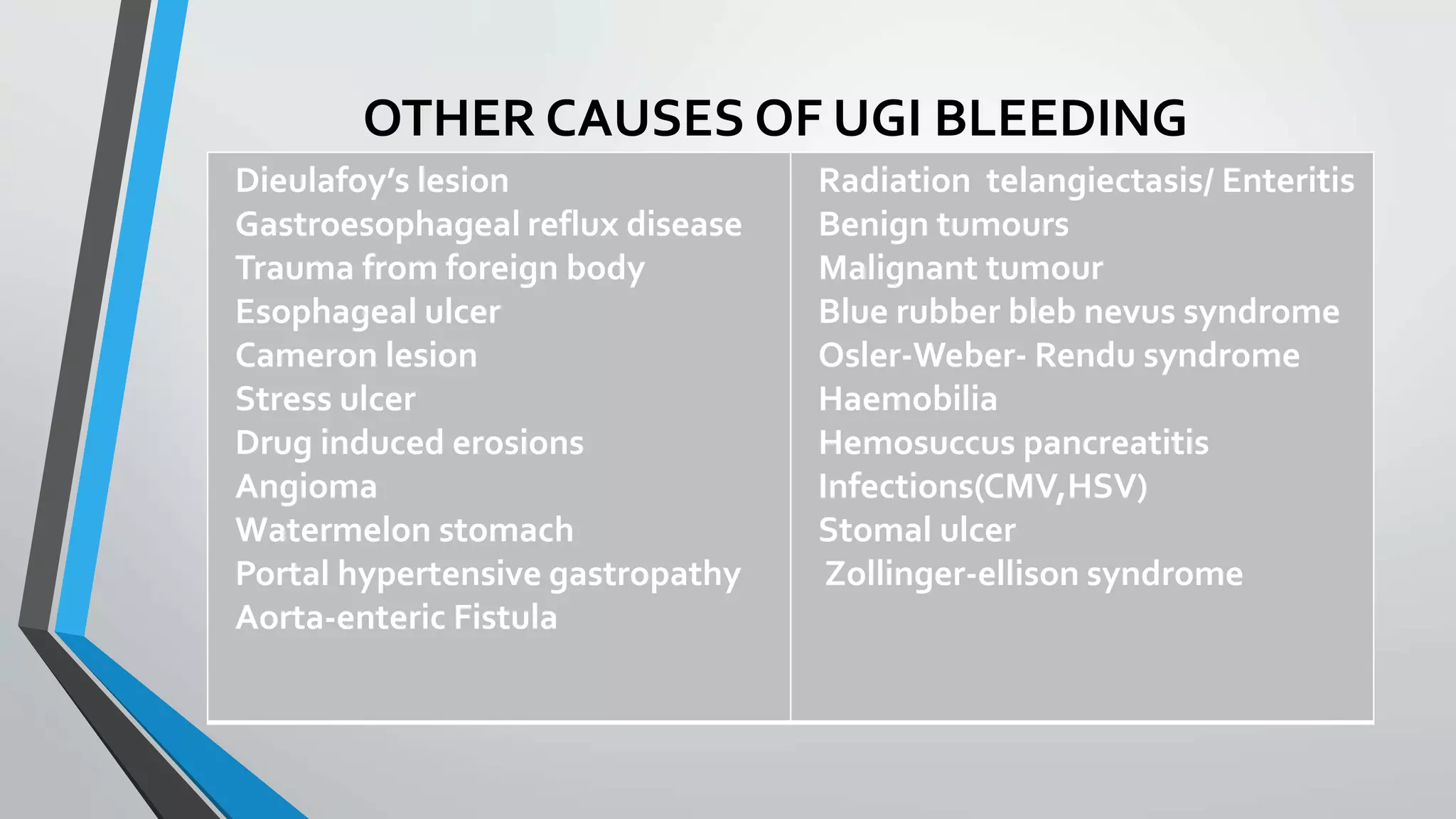
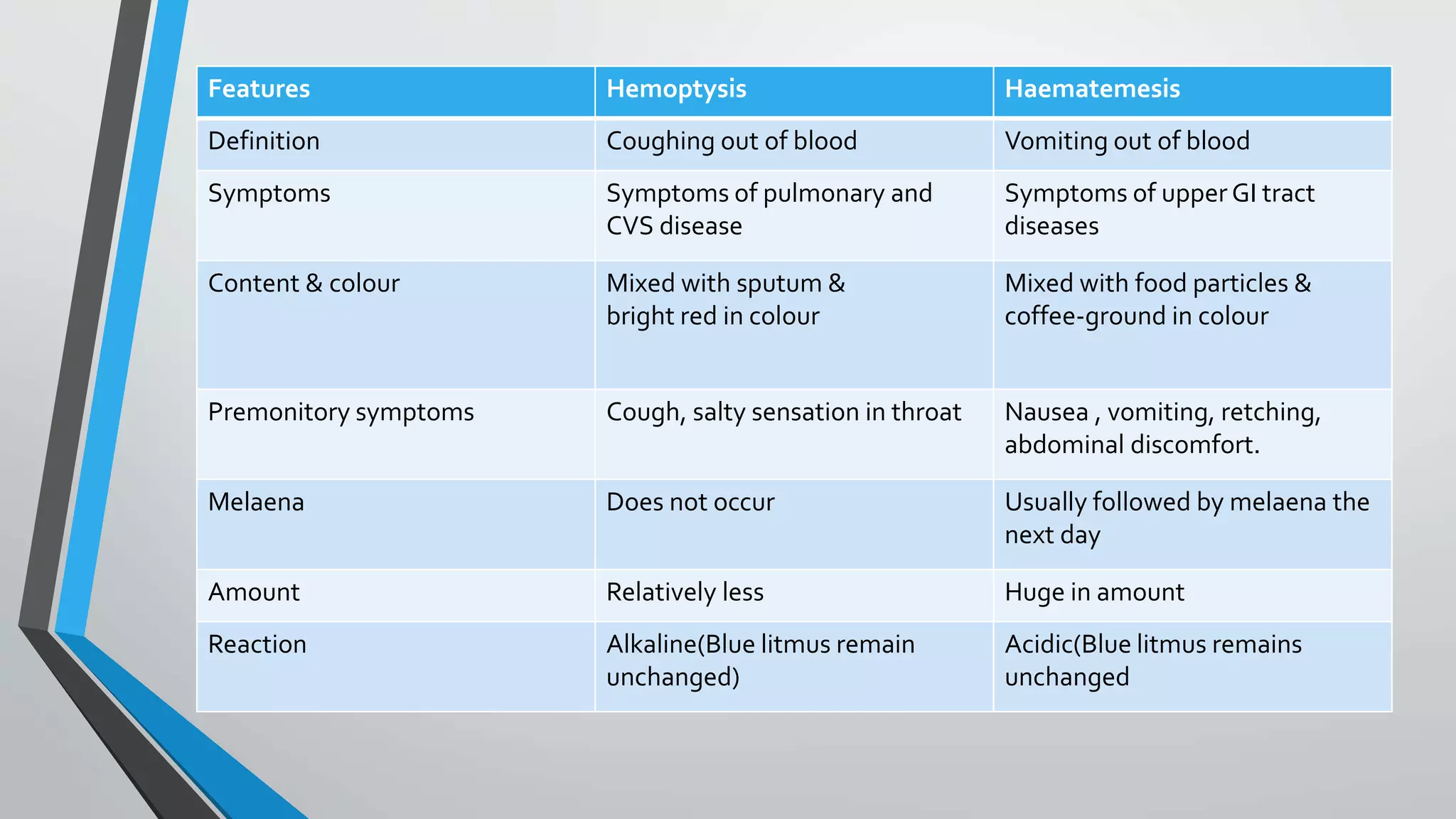
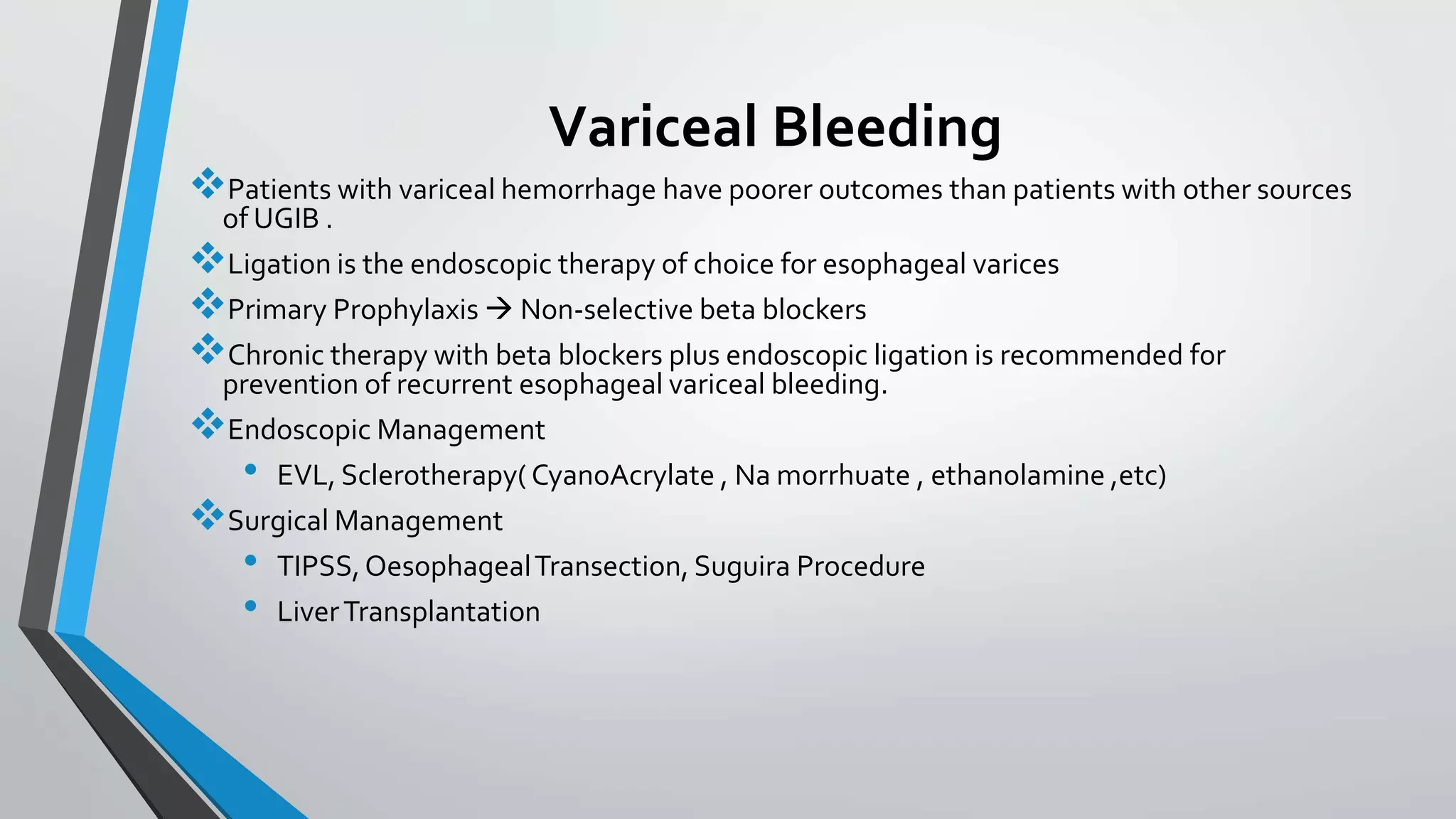
This document discusses the approach to patients with upper gastrointestinal bleeding and its management. It covers the following key points in 3 sentences:
The document outlines sources of GI bleeding, signs of blood loss severity, immediate assessment steps, diagnostic testing, endoscopic treatment options for variceal and non-variceal bleeding, risk stratification tools like the Rockall score, and angioembolization as a treatment option. Management involves fluid resuscitation, identifying the bleeding source, stopping active bleeding endoscopically, treating underlying causes, preventing rebleeding, and considering a second look endoscopy or other interventions based on risk stratification. Outpatient management may be appropriate for low risk patients while higher risk patients require intensive