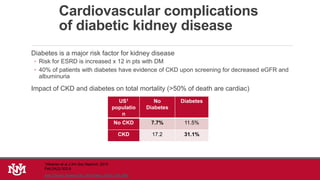
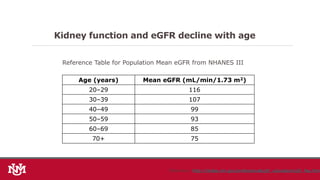
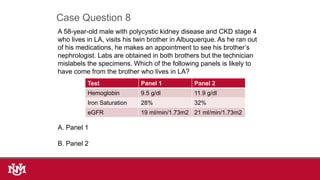
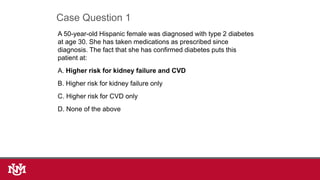
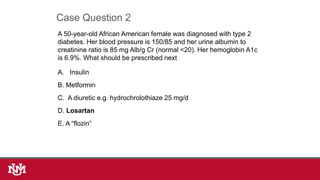
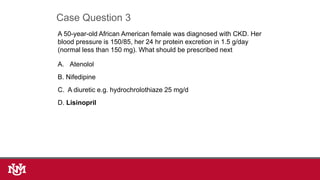
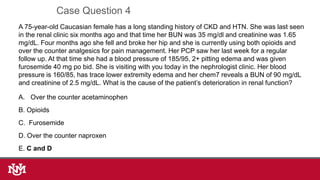
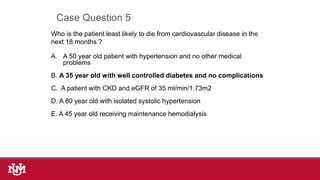
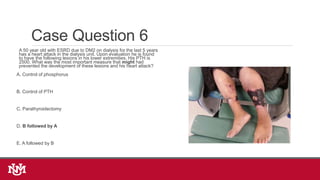
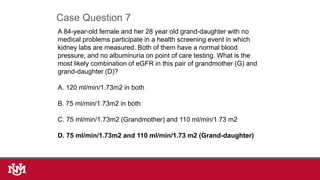
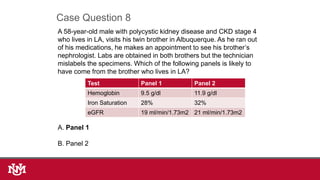
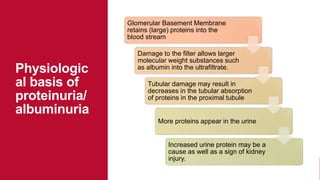
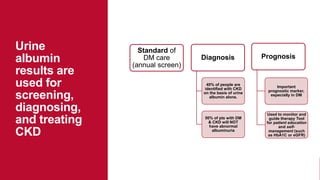
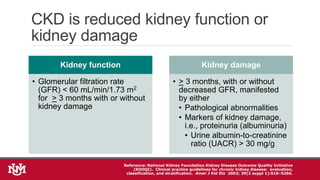
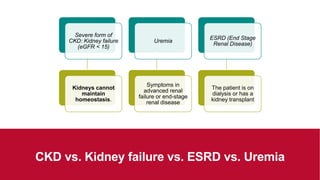
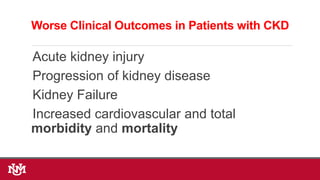
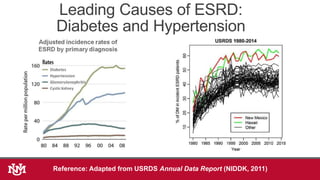
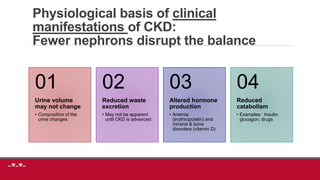
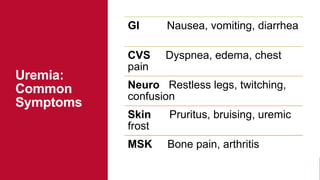
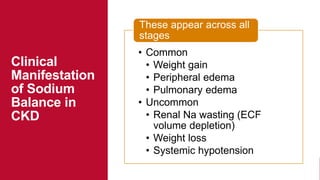
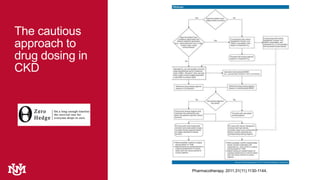
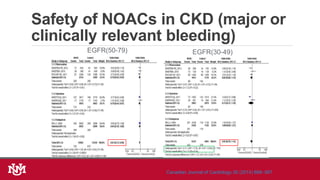
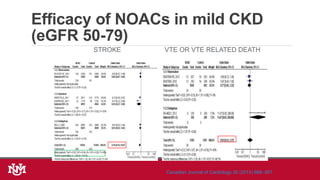
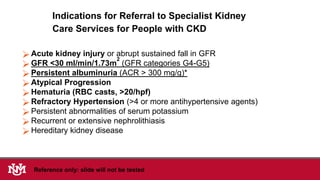
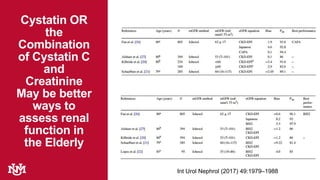
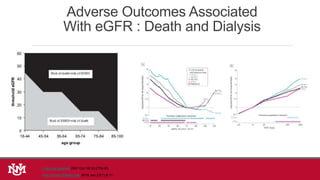
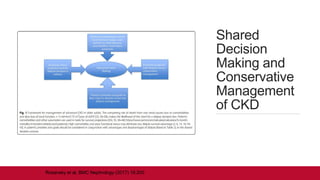
The document provides a comprehensive overview of chronic kidney disease (CKD), including its definition, assessment methods, epidemiology, clinical manifestations, and management strategies. It emphasizes the importance of early detection, particularly in special populations such as geriatric patients and those with diabetes, and outlines guidelines for treatment and referral to specialist care. Additionally, it addresses pharmacotherapy considerations and the impact of CKD on overall health outcomes.




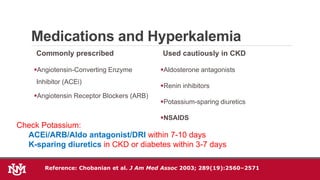
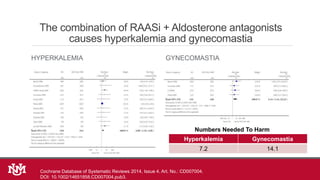
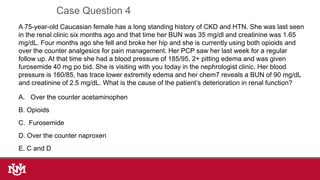
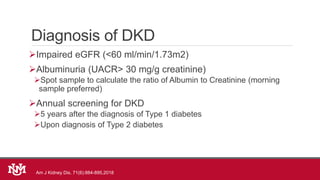
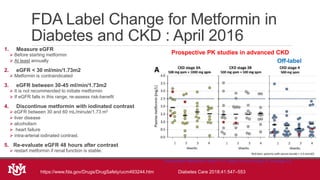
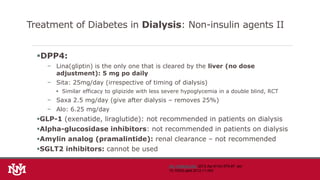
![Management of Hyperkalemia
o Reduce dietary potassium
o Stop medications causing hyperkalemia [NSAIDs, COX-2 inhibitors,
potassium sparing diuretics (aldactone)]
o Stop or reduce beta-blockers, ACEi/ARBs
o Avoid salt substitutes that contain potassium
o Use diuretics to increase renal potassium excretion
o Use Potassium binding resins (patiromer, ZS9)
1) Mahajan, et al. Kidney Int. 2010;78:303-309.
2) de Brito-Ashurst I, et al. J Am Soc Nephrol. 2009;20:2075-2084.
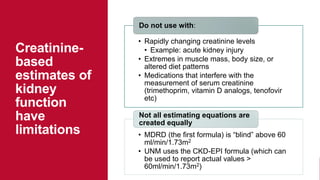
Things to remember in CKD : drugs that cause hyperkalemia (previous slide), measurement of
renal function 10 days after ACEI/ARB (for K and Renal Artery Stenosis) general principles of
management of hyperkalemia](https://image.slidesharecdn.com/ckdv2019app-191211133322/85/Chronic-Kidney-Disease-Update-2019-32-320.jpg)




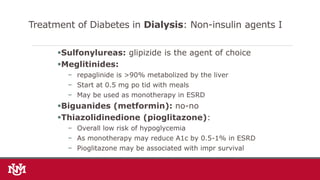
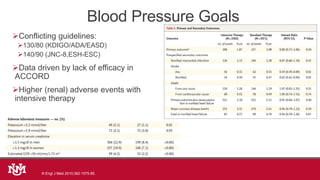
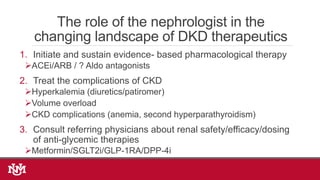
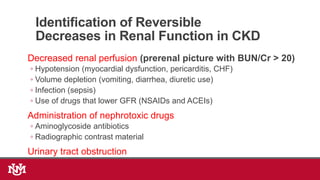
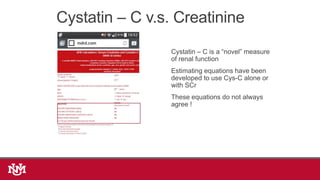
![The combination of RAASi + Aldosterone antagonists
improves proteinuria and blood pressure control
PROTEINURIA SYSTOLIC BLOOD PRESSURE
Diastolic BP: -1.73 [ -2.83, -0.62 ]
Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No.: CD007004.
DOI: 10.1002/14651858.CD007004.pub3.
eGFR -2.55 [ -5.61, 0.51 ] (favors SPL, NS)](https://image.slidesharecdn.com/ckdv2019app-191211133322/85/Chronic-Kidney-Disease-Update-2019-72-320.jpg)