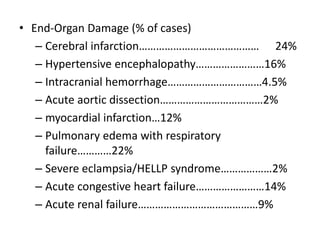
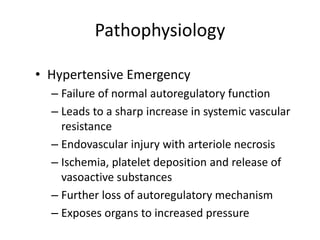
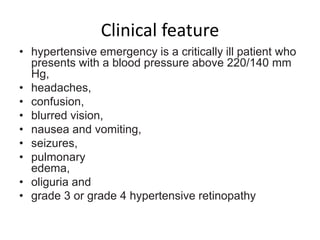
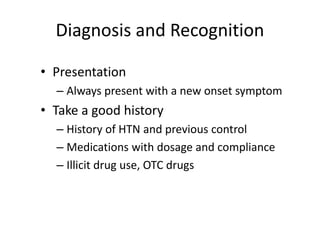
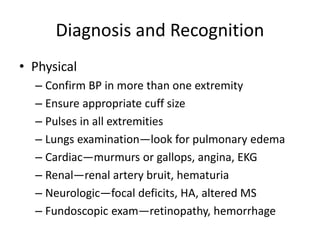
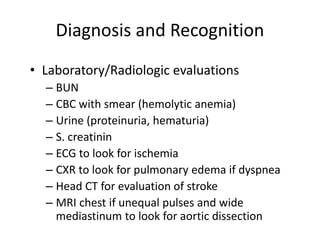
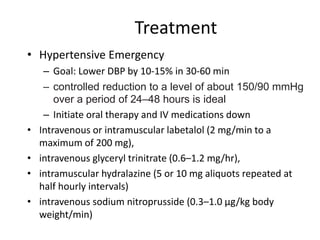
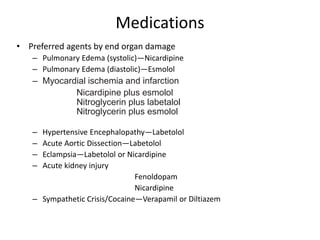
This document discusses hypertensive encephalopathy and hypertensive emergencies. It defines hypertensive encephalopathy as a condition caused by very high blood pressure that results in neurological symptoms. It describes the pathogenesis, symptoms, investigations, diagnosis, and treatment, which involves slowly lowering blood pressure over 24-48 hours. Hypertensive emergencies involve acute severe blood pressure elevations that cause end organ damage and require admission and rapid blood pressure control within hours to prevent further damage. The document outlines the clinical features, diagnosis, and treatments for hypertensive emergencies depending on the affected organ.