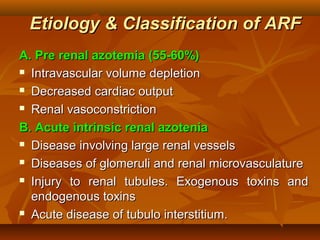
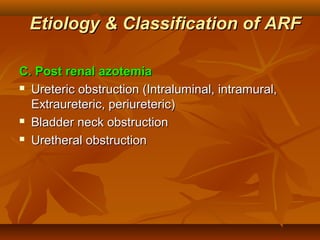
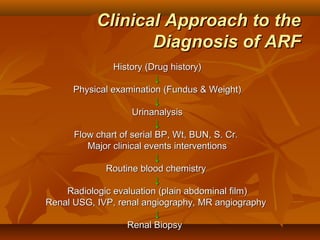
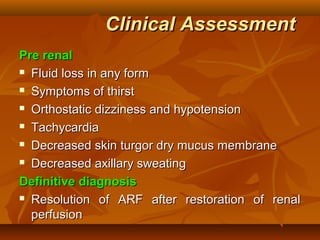
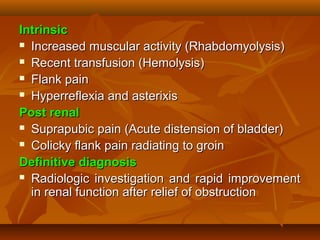
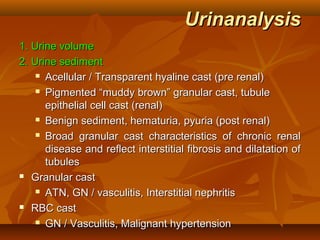
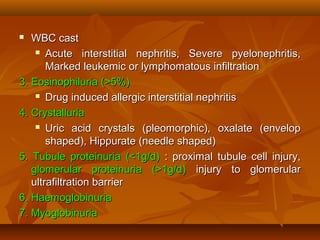
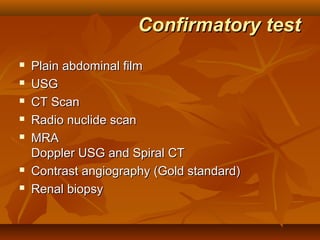
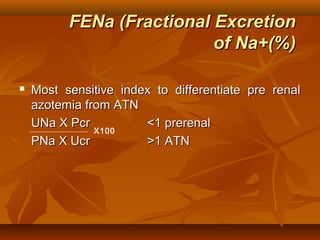
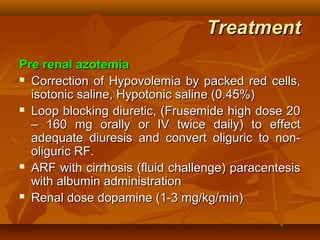
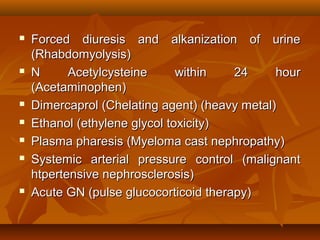
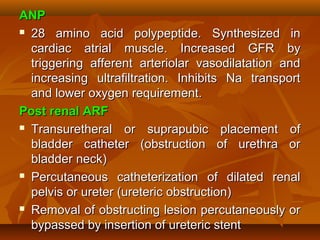
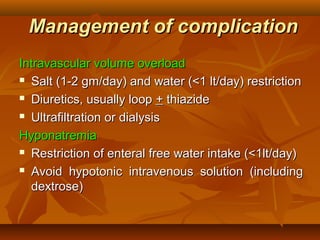
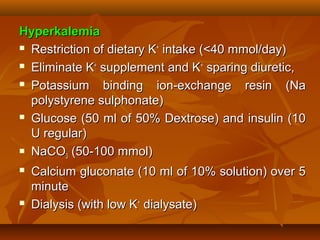
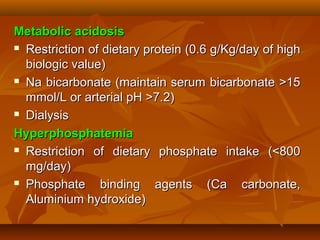
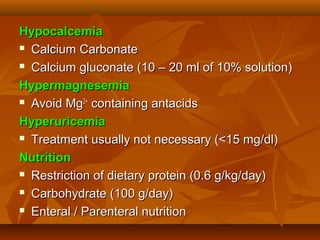
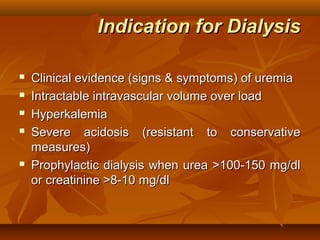
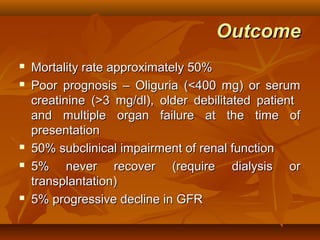
The document discusses the management of acute renal failure (ARF), outlining its definition, etiology, classification, diagnostic approach, and treatment strategies. It details the causes of pre-renal, intrinsic, and post-renal azotemia, along with clinical assessment techniques and laboratory tests necessary for diagnosis. Additionally, it addresses the management of complications and the indications for dialysis, highlighting the overall mortality rate and prognosis for patients with ARF.