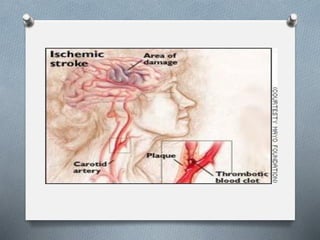
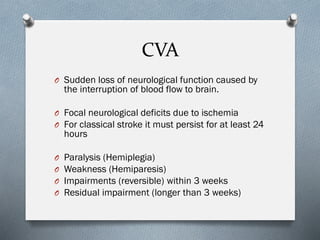
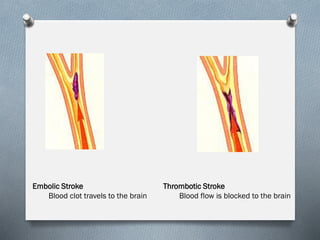
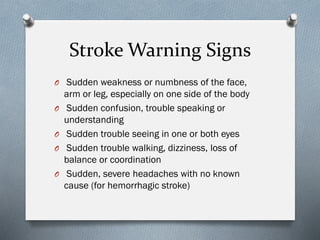
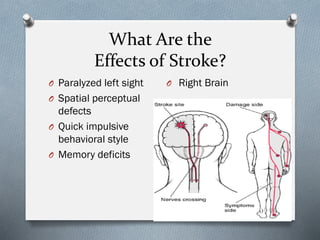
Stroke occurs when blood flow to the brain is interrupted, and there are two main types: ischemic (caused by blockage) and hemorrhagic (caused by bleeding). Stroke is a leading cause of long-term disability and death in the United States. Risk factors include high blood pressure, heart disease, smoking, and diabetes. Treatment depends on the type of stroke, but may involve clot-busting drugs or surgery to repair damaged blood vessels. Rehabilitation is important for recovery and aims to restore functions like movement, speech, and daily living skills through therapies.