This document discusses brain death, including its historical definition, current diagnostic criteria, pathophysiology, and management of organ donors. Key points include:
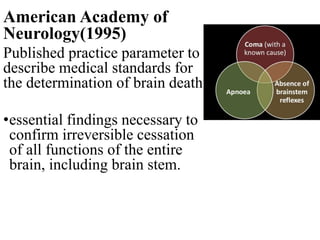
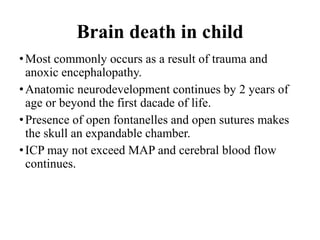
- Brain death is defined as irreversible cessation of all functions of the entire brain, including the brain stem.
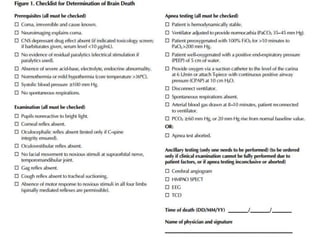
- Diagnosis requires two examinations at least 6 hours apart showing coma, absence of brainstem reflexes, and apnea during a standardized test. Ancillary tests like EEG can be used if clinical criteria are inconclusive.
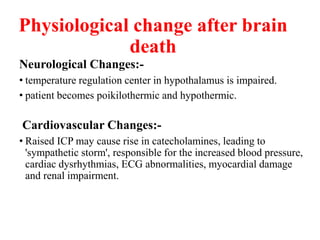
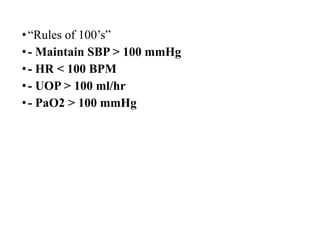
- After brain death, pathophysiological changes occur like hypotension, diabetes insipidus, and coagulopathies due to loss of autonomic and endocrine functions regulated by the brain.