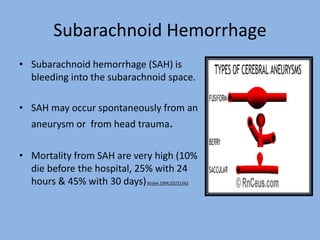
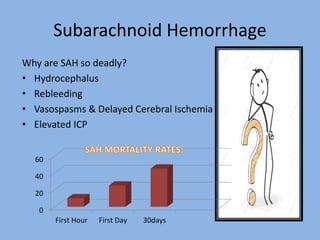
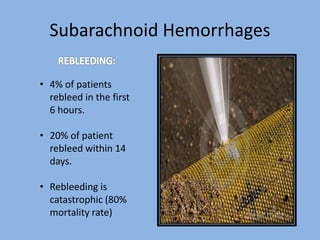
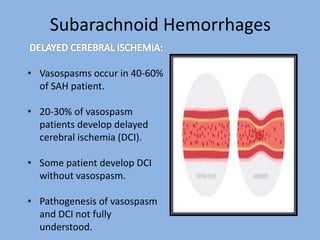
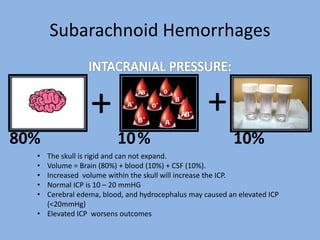
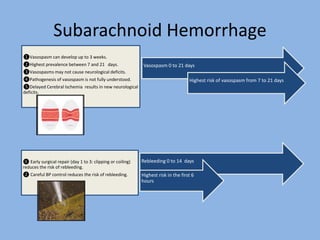
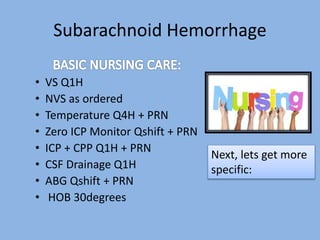
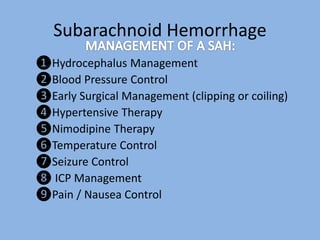
Subarachnoid hemorrhage occurs when there is bleeding into the subarachnoid space surrounding the brain. It carries a high mortality rate, with 10% dying before reaching the hospital and up to 45% dying within 30 days. Rebleeding and development of vasospasms are major risks that can lead to elevated intracranial pressure, cerebral ischemia, and neurological deficits. Aggressive management including early aneurysm repair, careful blood pressure control, nimodipine therapy, and ICP monitoring is required to prevent rebleeding and mitigate risks of vasospasms and cerebral ischemia.