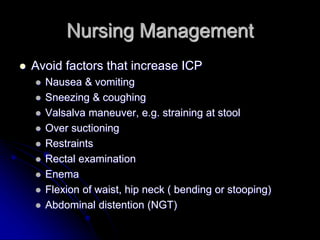
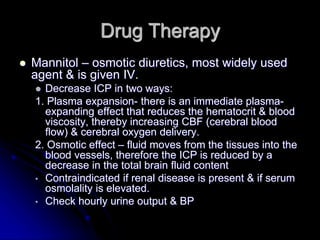
This document discusses increased intracranial pressure. It can result from an increase in brain tissue, blood, or cerebrospinal fluid within the skull. Common causes include head injuries, brain tumors, strokes, and hydrocephalus. Symptoms include restlessness, changes in consciousness, changes in vital signs, headaches, nausea, vomiting, pupil changes, and decreased motor function. Treatment involves managing symptoms, monitoring intracranial pressure, administering medications to reduce pressure such as mannitol and diuretics, and surgical intervention if needed.