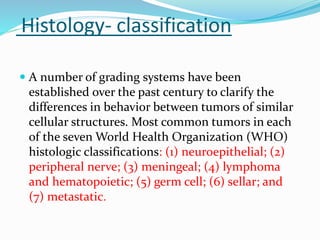
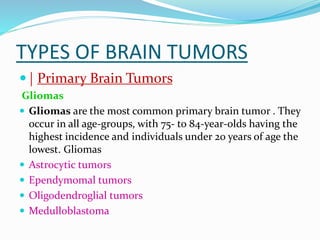
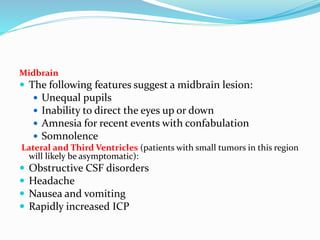
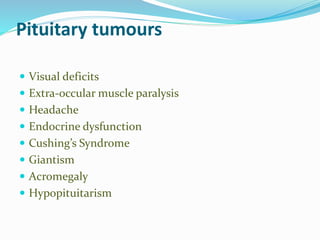
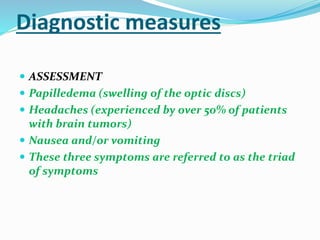
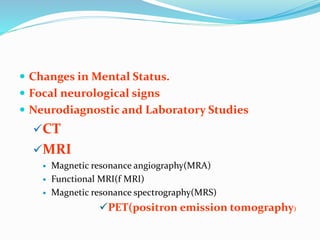
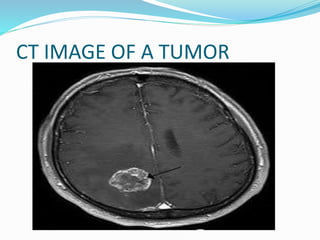
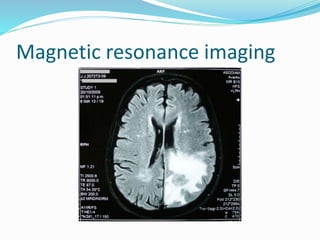
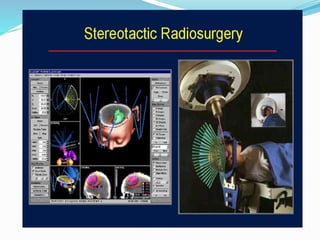
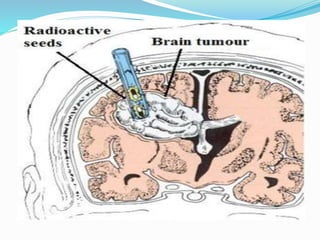
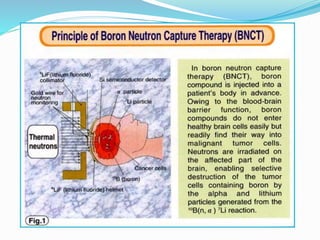
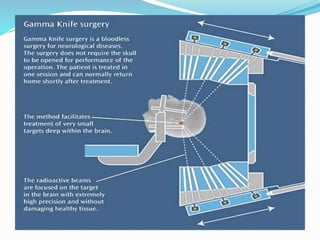
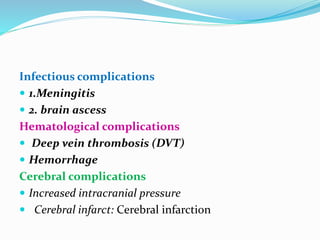
This document provides information on intracranial space occupying lesions including classification, types of brain tumors, clinical manifestations, diagnostic measures, treatment options including surgery, radiation and chemotherapy, as well as postoperative complications. It classifies lesions as congenital, traumatic, inflammatory, parasitic or neoplastic and describes common tumor types such as gliomas, meningiomas and pituitary adenomas. Diagnostic tools include CT, MRI, PET and biopsy. Treatment involves surgery, radiation including gamma knife and brachytherapy, as well as chemotherapy.