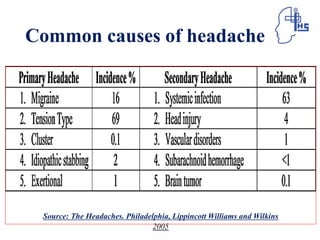
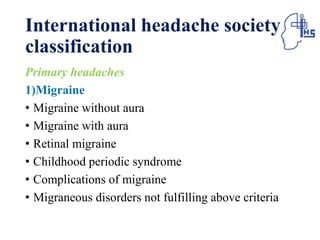
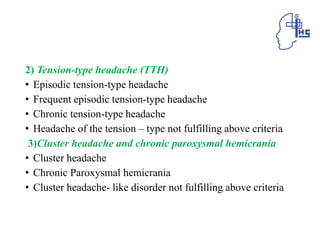
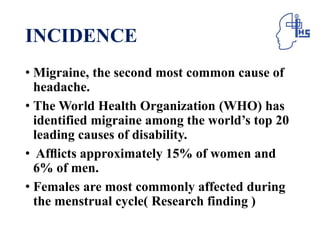
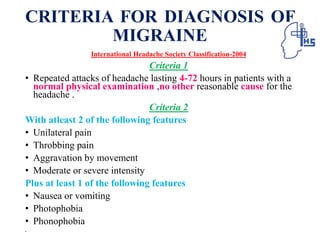
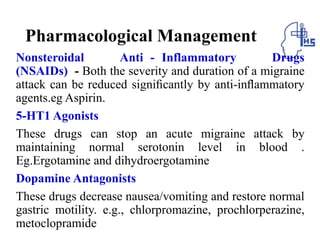
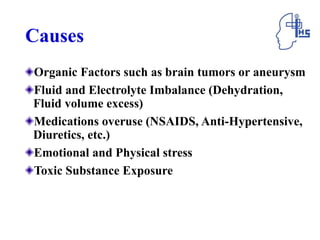
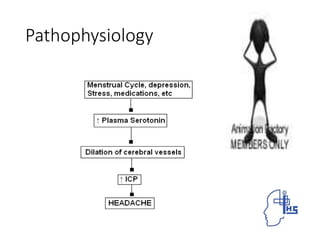
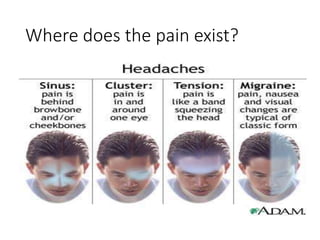
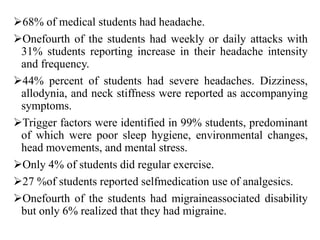
The document provides information on different types of primary headaches including migraine, tension-type headache, and cluster headache. It defines migraine as a recurrent throbbing headache affecting one side of the head that is often accompanied by nausea and visual disturbances. Tension-type headache is described as a chronic pain syndrome characterized by bilateral tight band-like discomfort. Cluster headache is defined as a rare but excruciating headache associated with autonomic symptoms like tearing and nasal congestion. The document discusses causes, symptoms, pathophysiology, diagnostic criteria and management of these primary headache types.