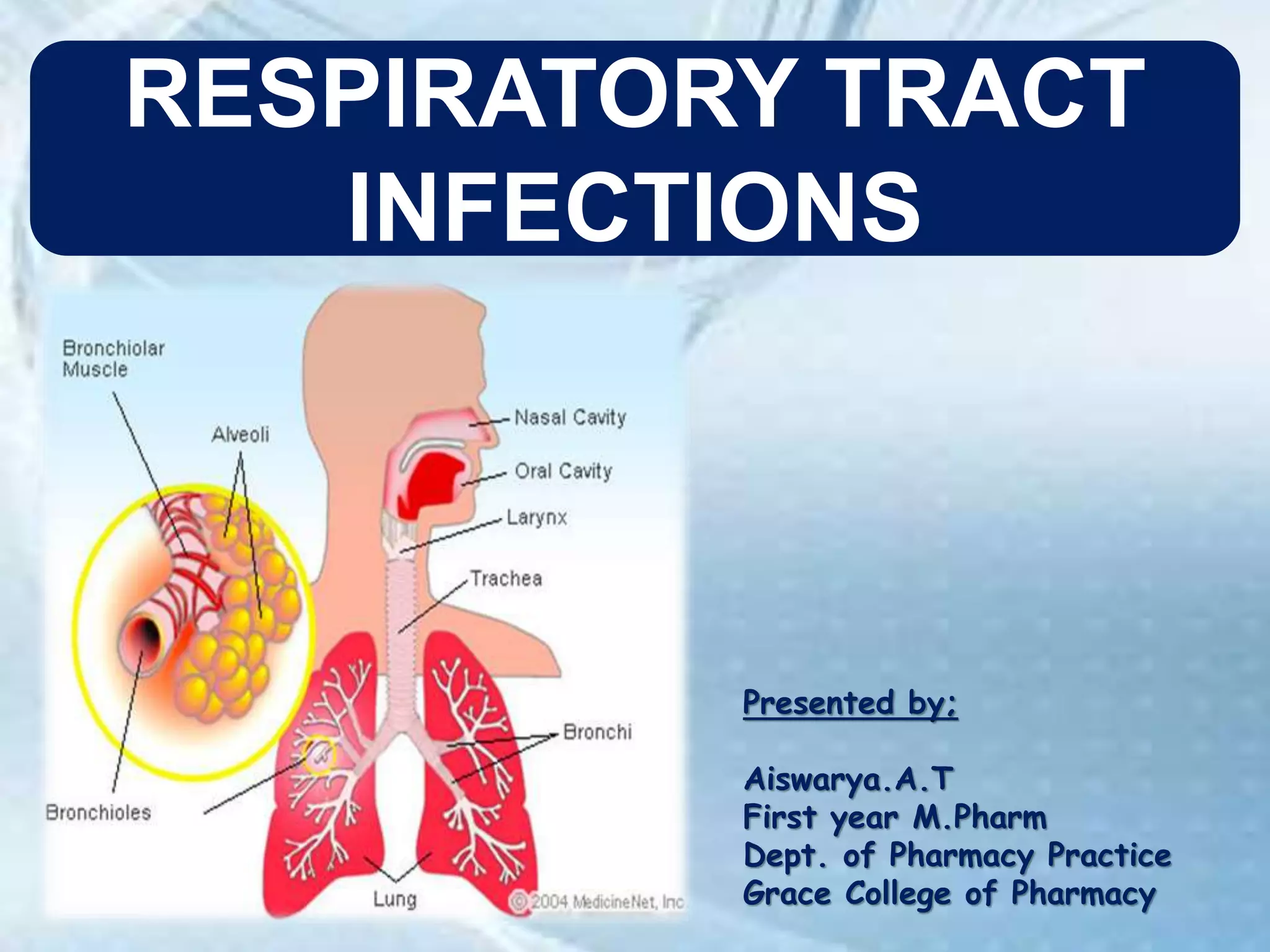
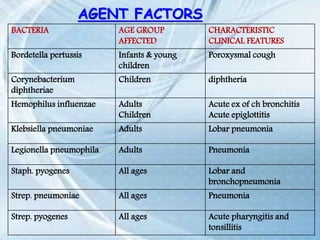
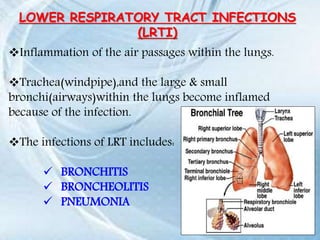
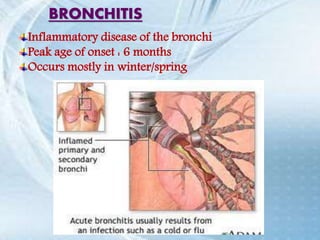
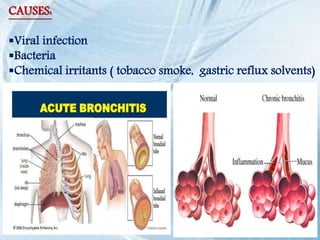
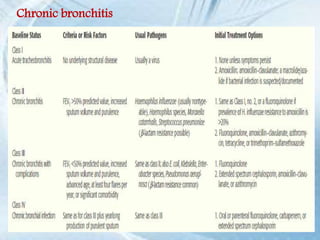
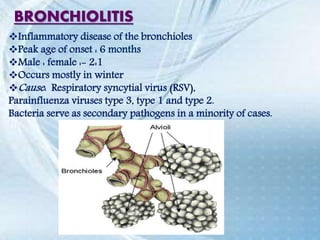
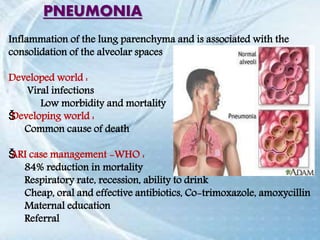
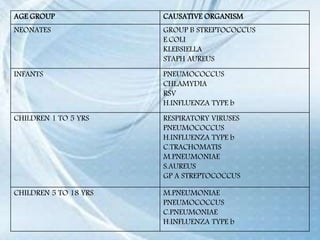
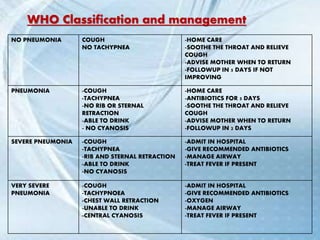
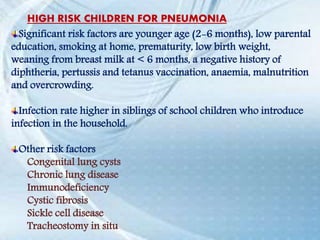
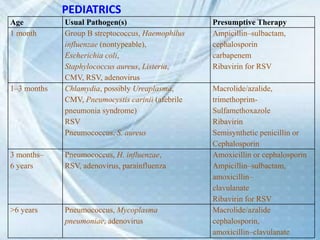
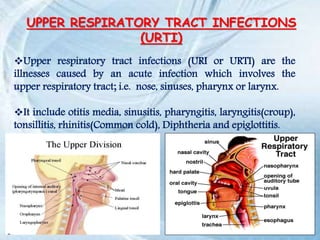
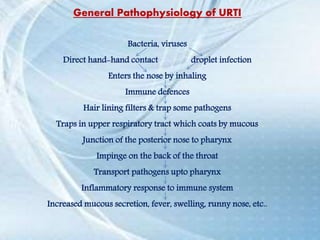
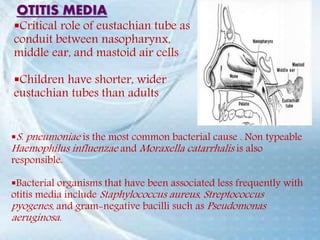
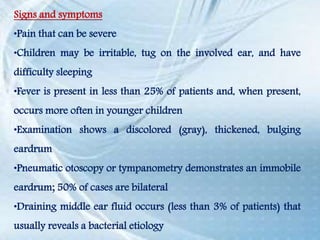
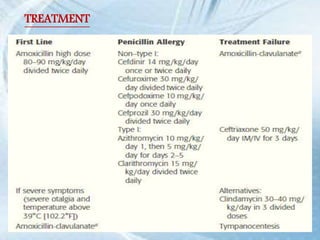
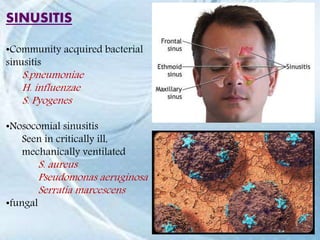
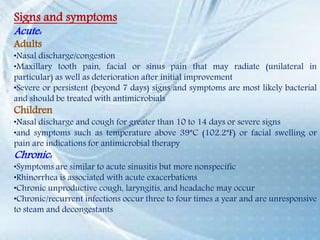
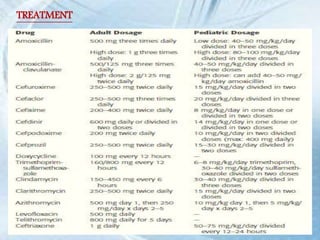
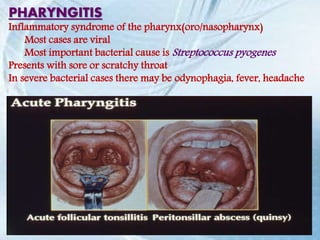
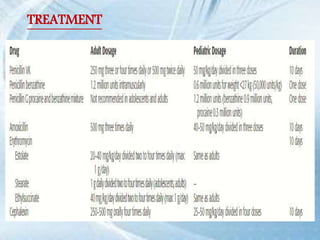
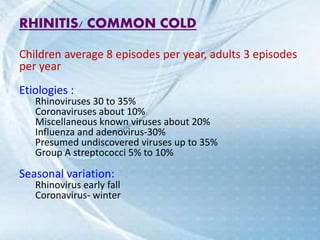
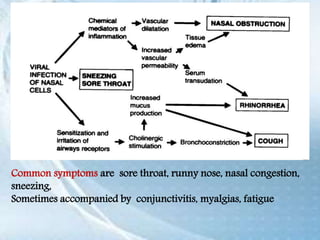
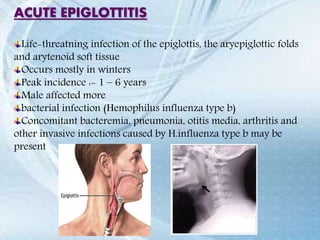
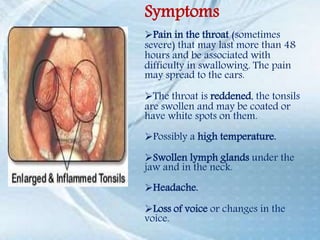
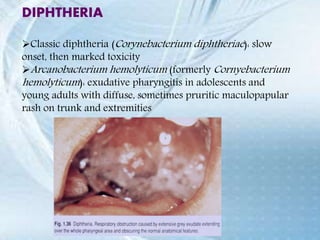
This document discusses respiratory tract infections, which are infections that involve the respiratory tract. It describes upper respiratory tract infections such as sinusitis, pharyngitis, and otitis media, and lower respiratory tract infections such as bronchitis, bronchiolitis, and pneumonia. For each infection, it discusses the typical causative agents, affected age groups, characteristics, clinical features, and treatment approaches. It provides an overview of the pathophysiology of upper and lower respiratory tract infections.