1. Pneumonia, lung abscess, and pleural effusion are respiratory infections that can affect the lungs. Pneumonia is an inflammation of the lung tissues that is usually caused by microorganisms. Lung abscess occurs when an area of lung tissue becomes necrotic and fills with pus. Pleural effusion is an excess collection of fluid in the pleural space surrounding the lungs.
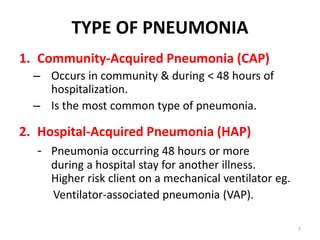
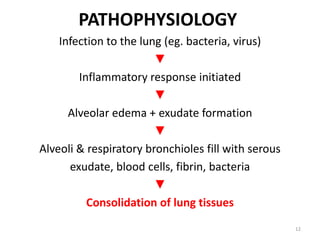
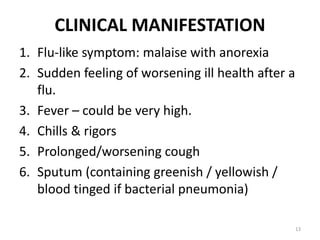
2. The document discusses the causes, pathophysiology, clinical manifestations, diagnosis, and treatment of each condition. It provides details on the different types of pneumonia and outlines strategies for educating clients to prevent respiratory infections.