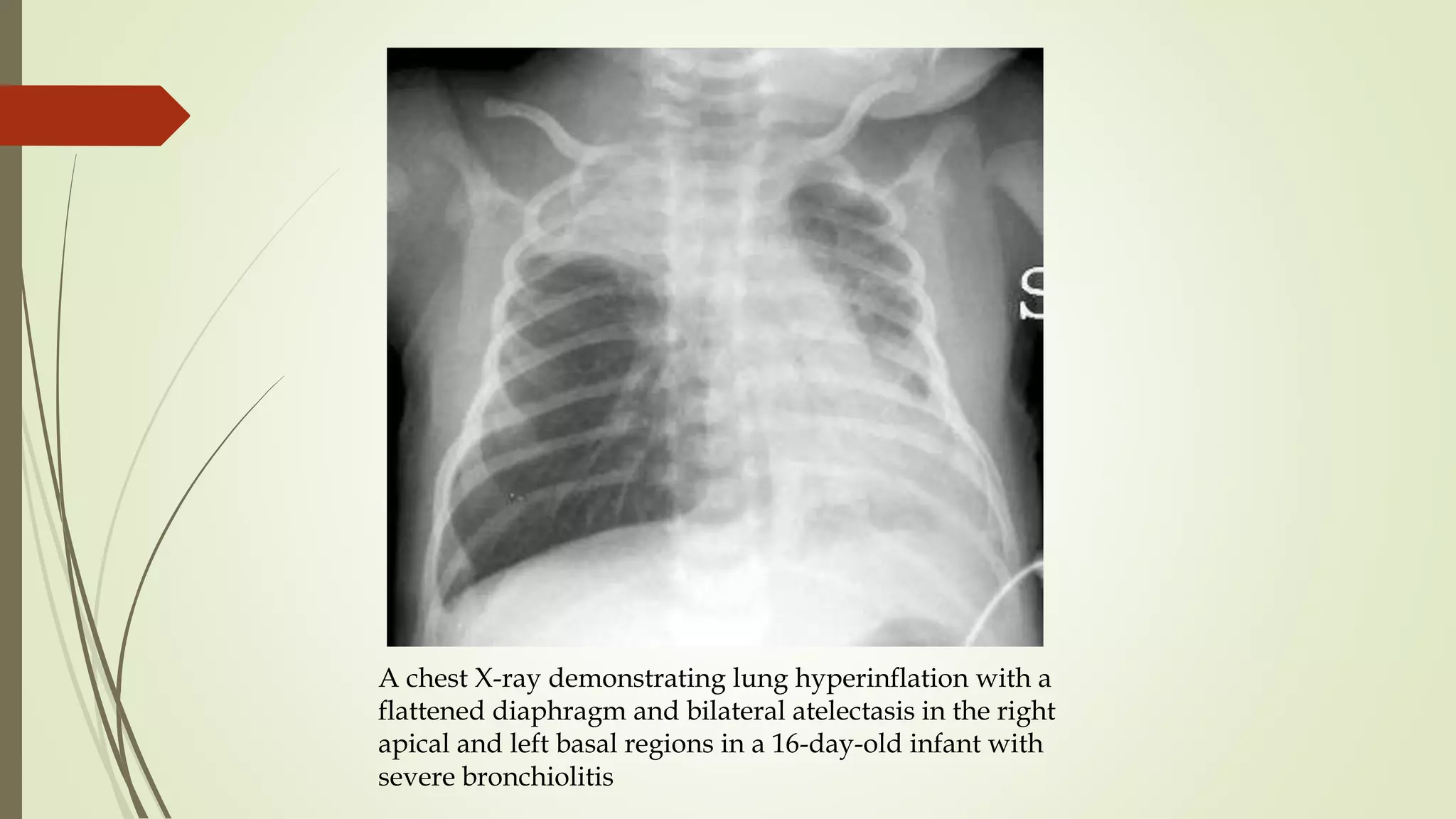
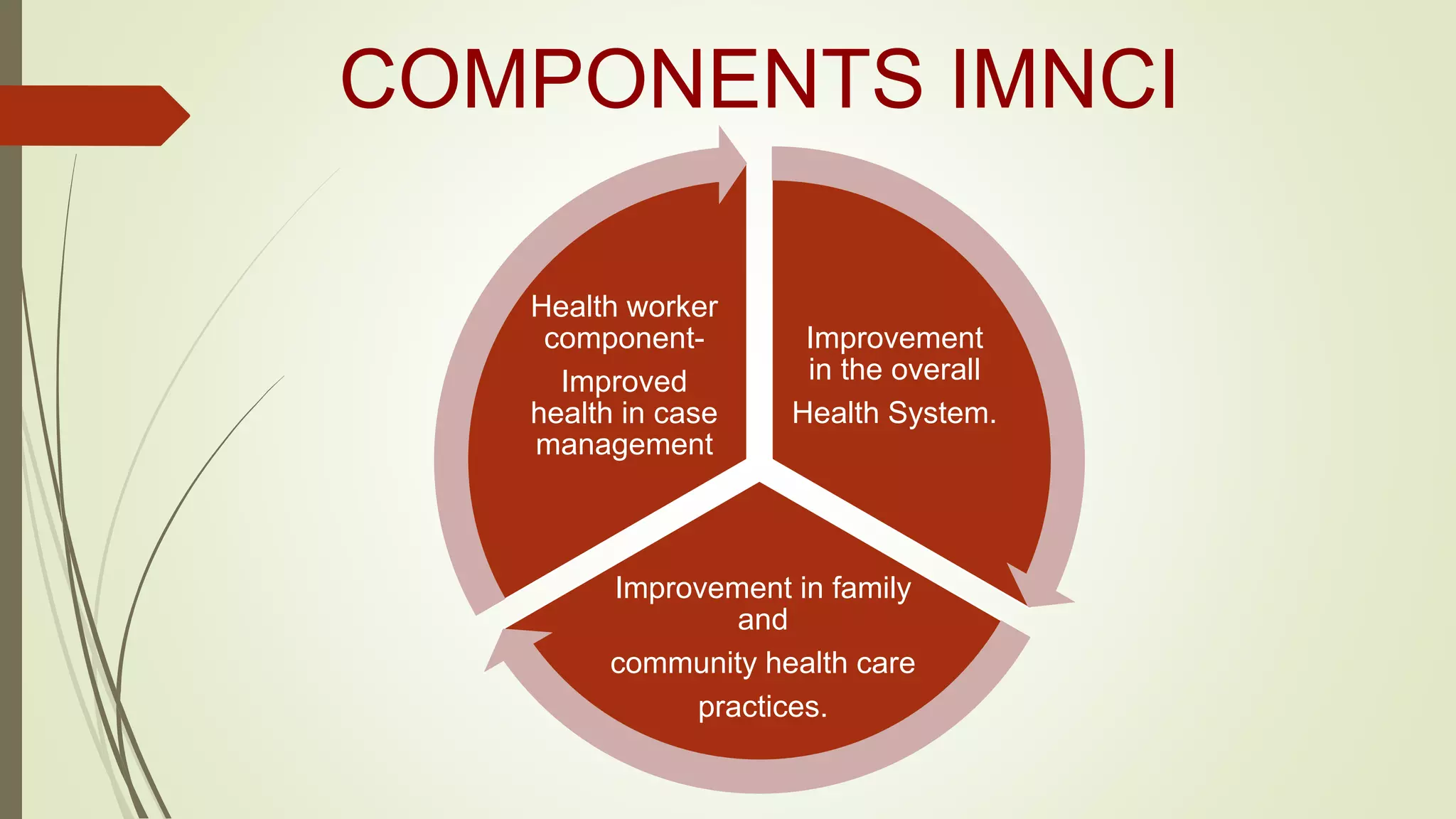
The document discusses acute respiratory infections (ARIs) in children, categorizing them into upper and lower respiratory infections, detailing their epidemiology, contributing factors, and treatment options. It highlights the common cold, tonsillitis, bronchiolitis, and pneumonia, emphasizing management techniques and preventative measures, particularly through integrated management strategies like IMNCI. The document aims to improve child health outcomes by addressing early diagnosis, treatment, and family education on health practices.