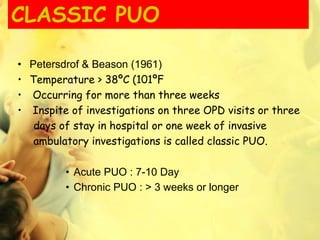
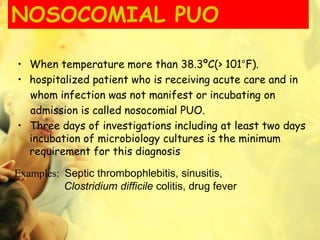
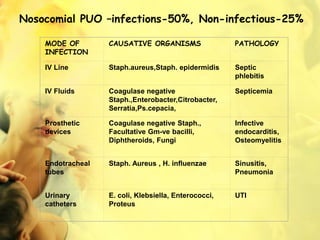
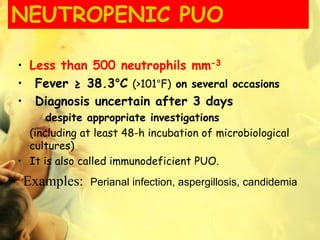
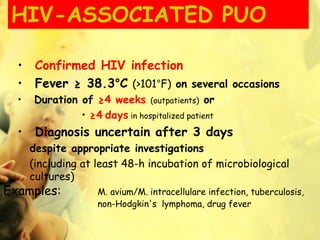
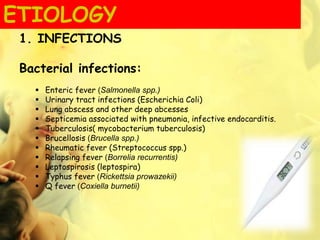
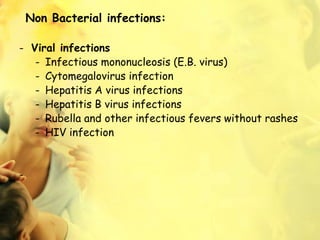
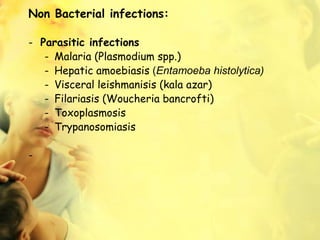
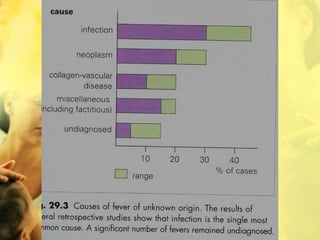
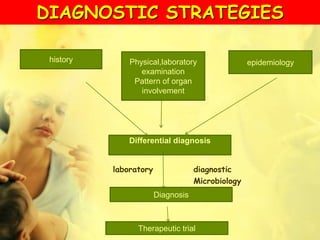
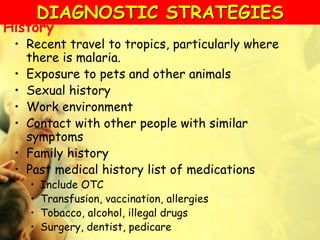
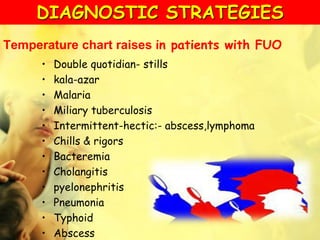
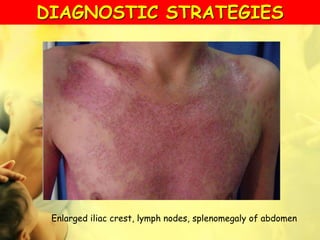
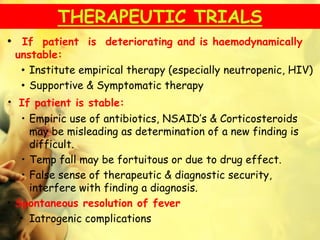
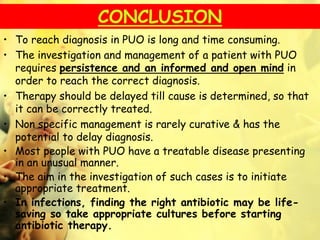
Pyrexia of unknown origin (PUO) is defined as a fever over 38°C lasting three weeks or longer without a diagnosis despite extensive investigation. There are various types of PUO, including classic, nosocomial, neutropenic, and HIV-associated, each with specific characteristics and diagnostic criteria. Effective management requires thorough diagnostic workup and ideally should delay therapy until the cause is identified to ensure the correct treatment.