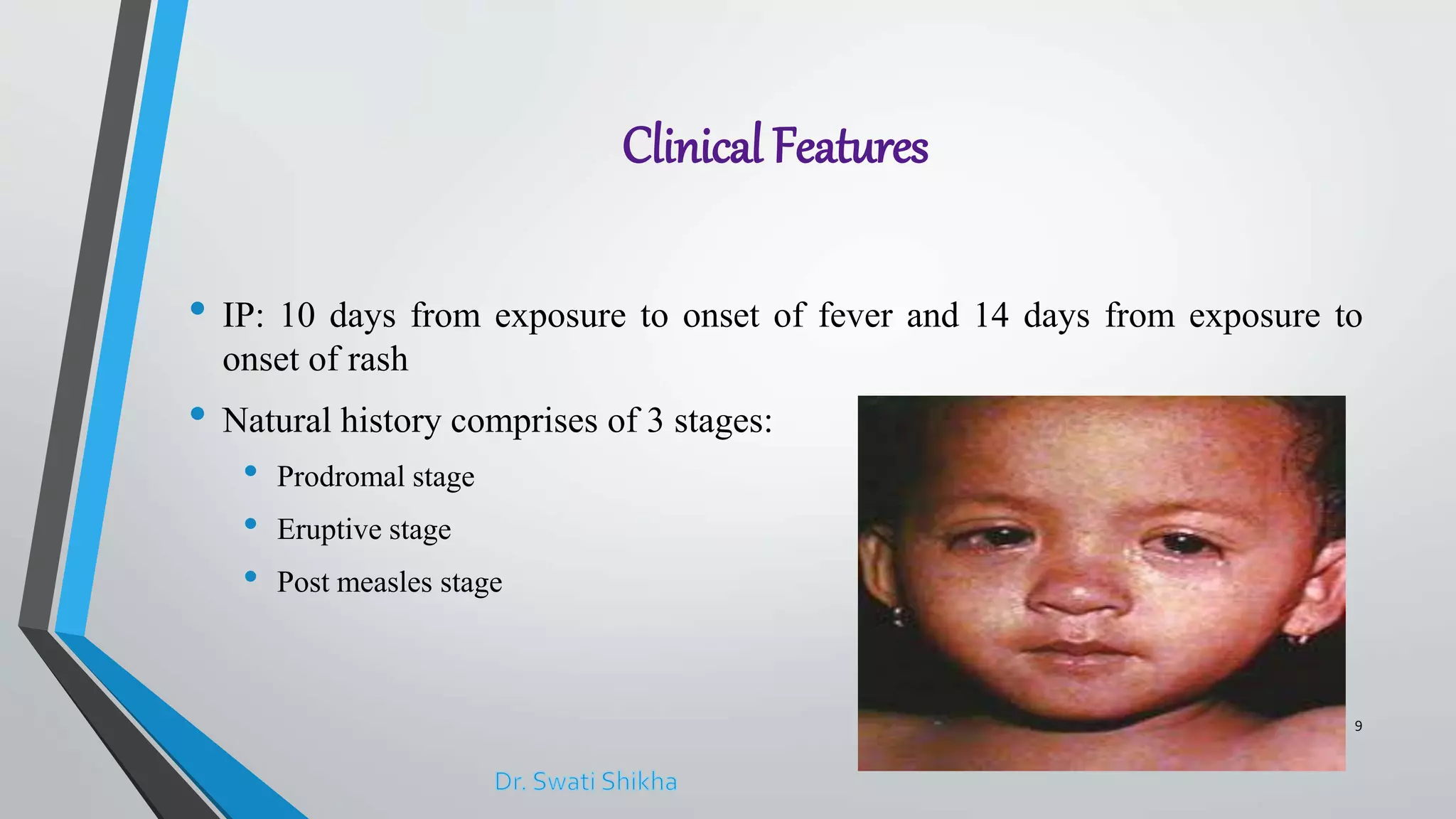
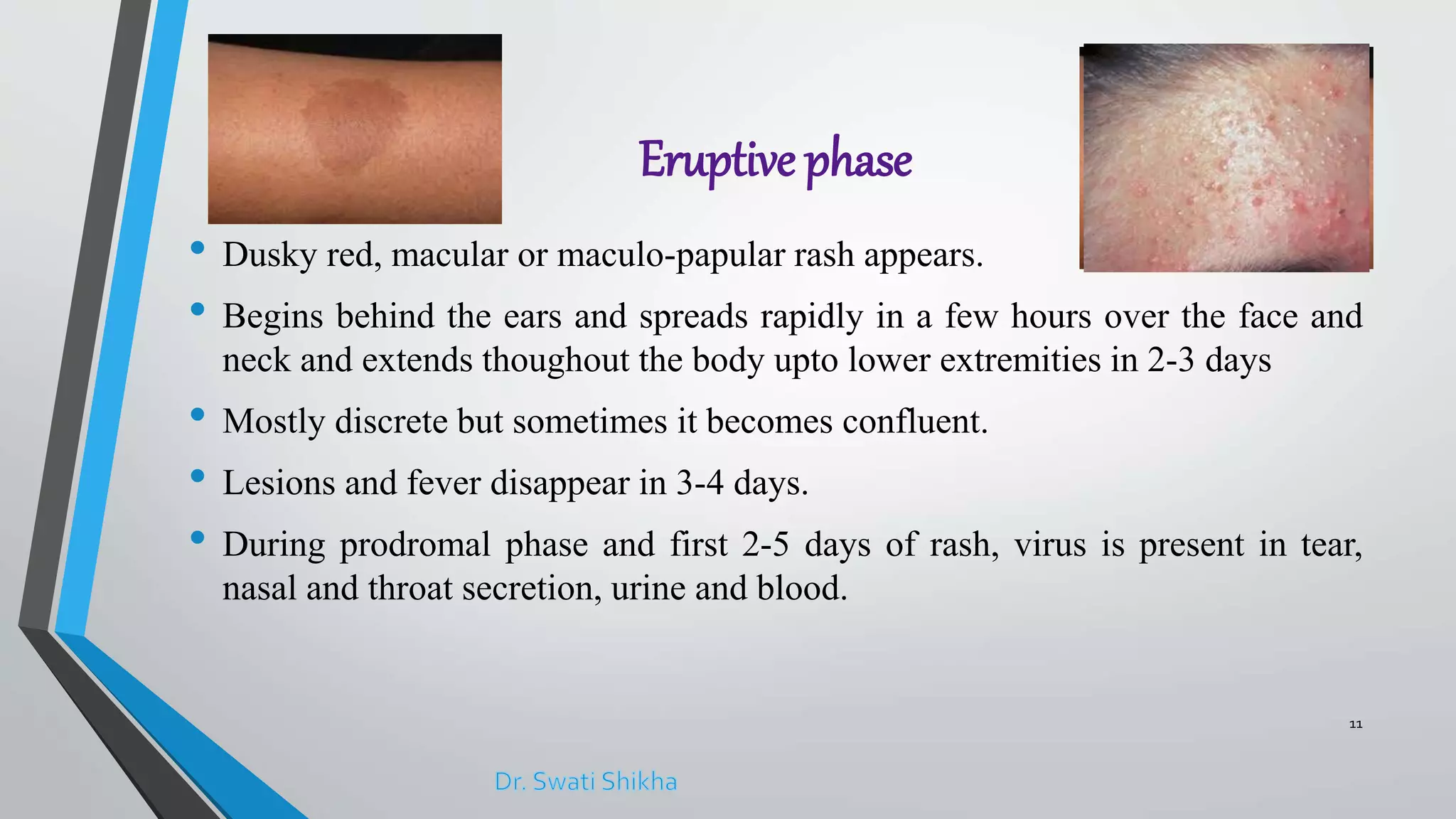
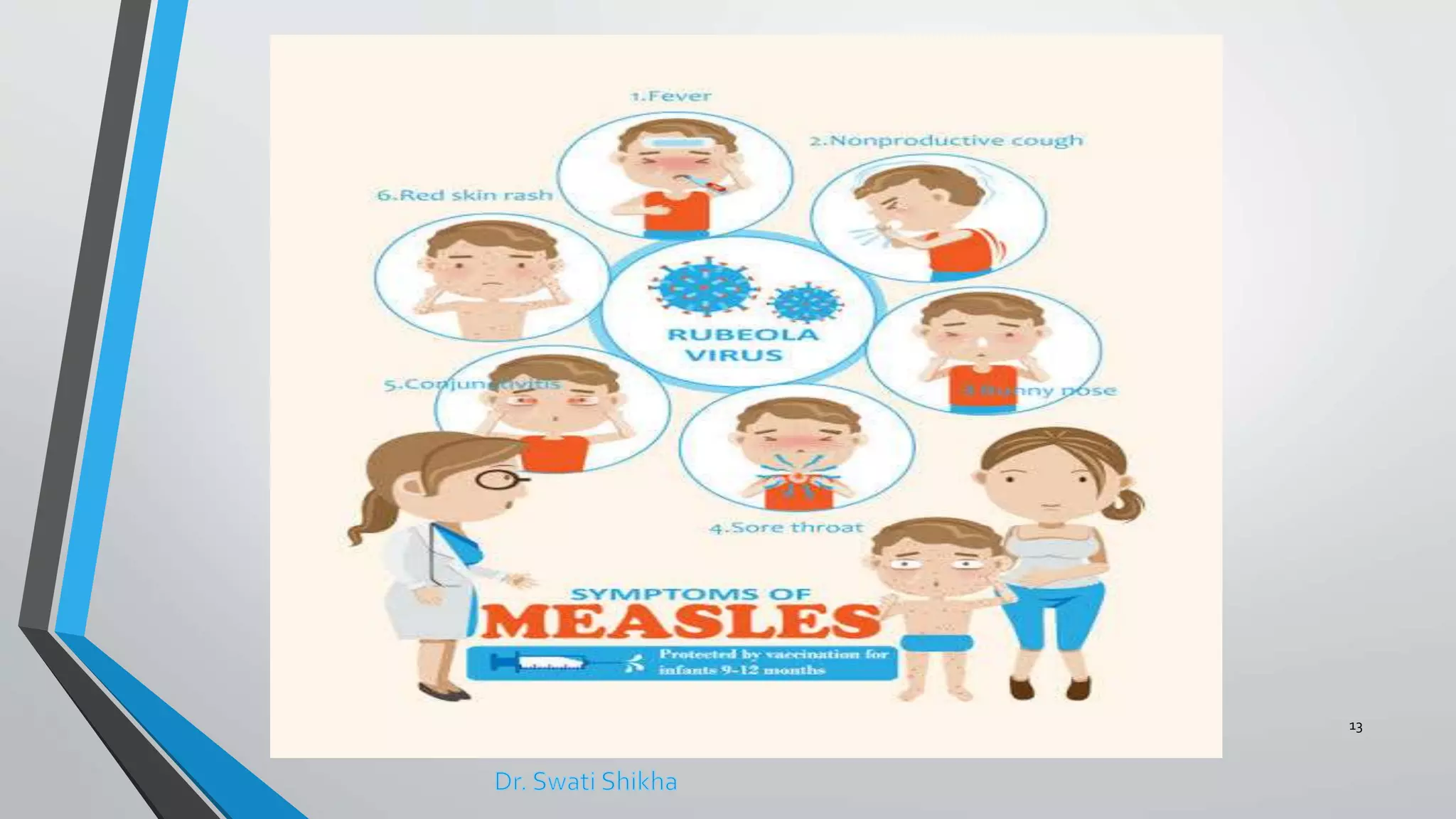
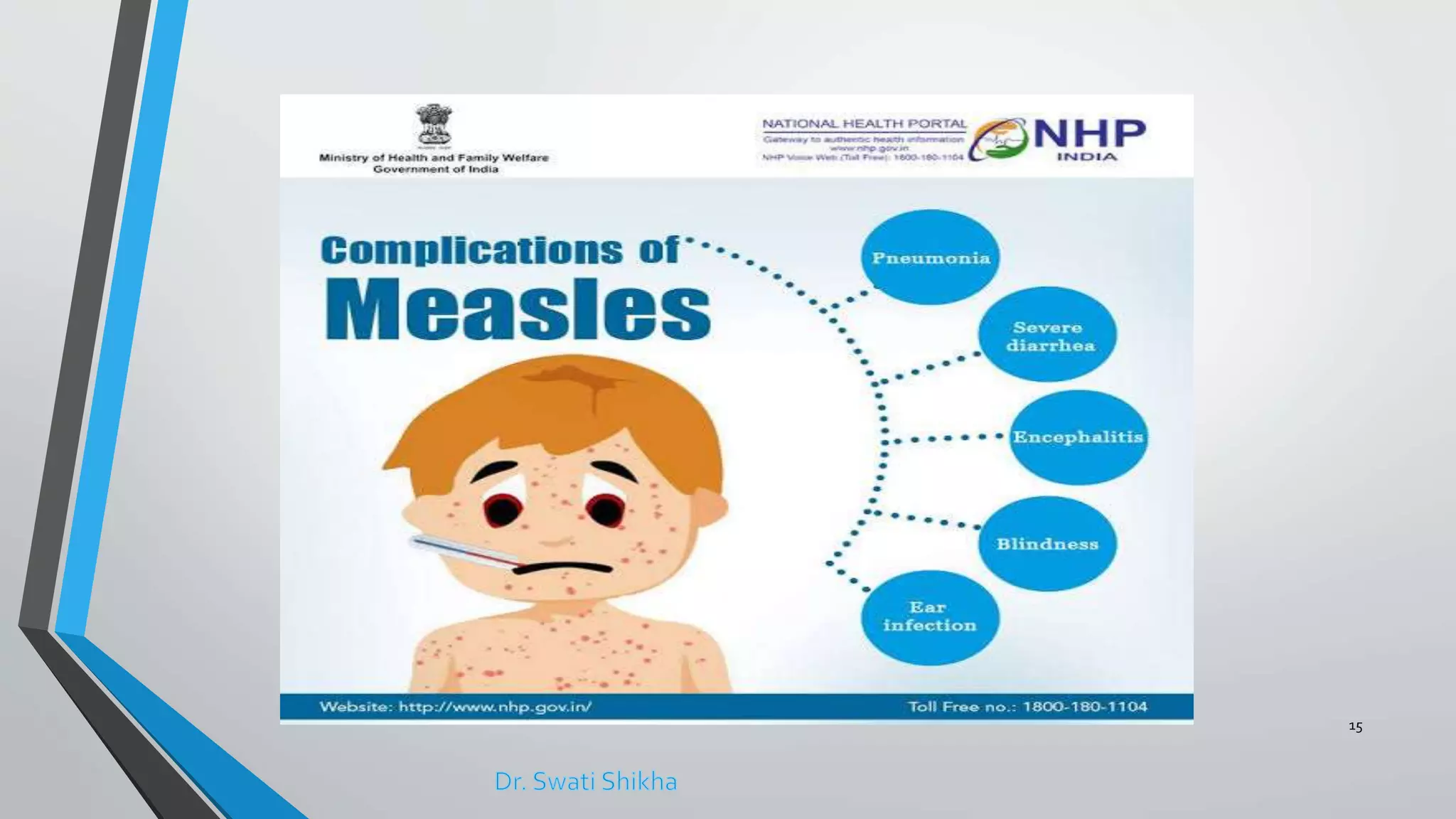
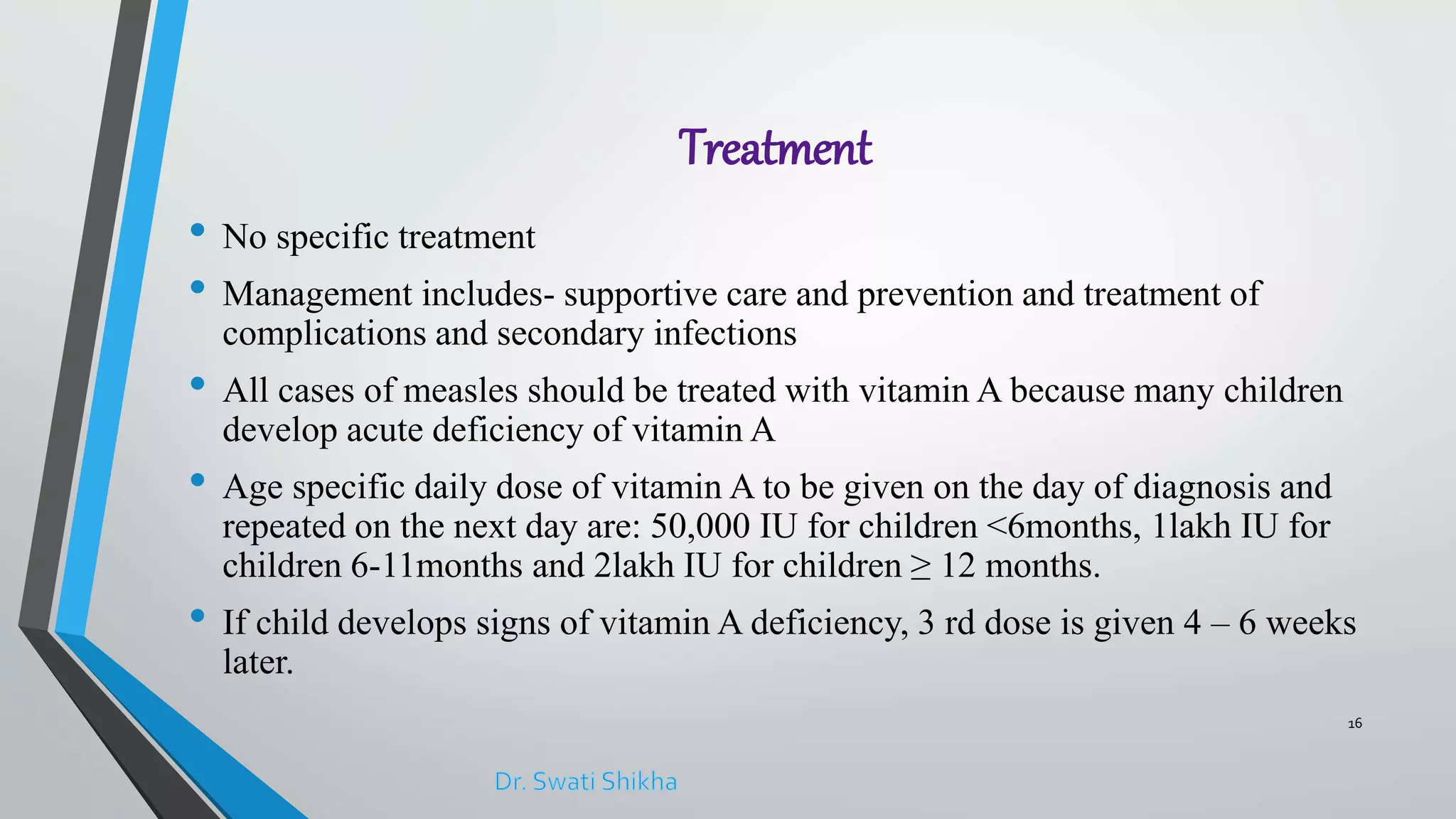
The document provides an overview of measles, detailing its epidemiology, clinical features, complications, treatment, and prevention strategies. It highlights the high infectious nature of the disease, particularly in developing countries, and discusses the challenges in eliminating it, such as weak immunization systems and increasing vaccine refusal. The document emphasizes the importance of vitamin A treatment for affected children and the role of vaccination in preventing measles.