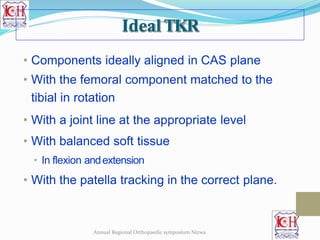
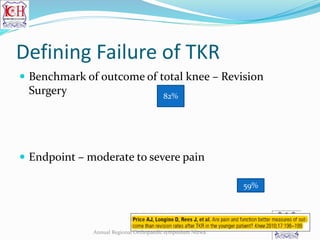
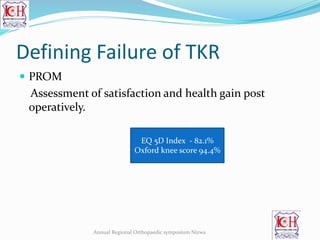
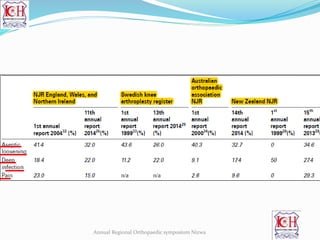
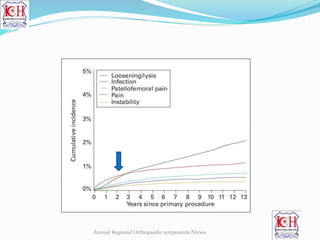
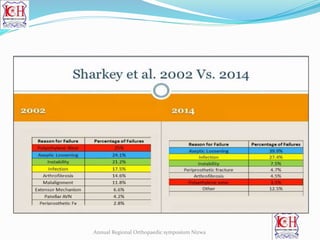
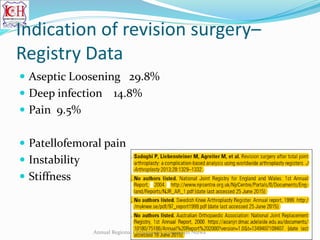
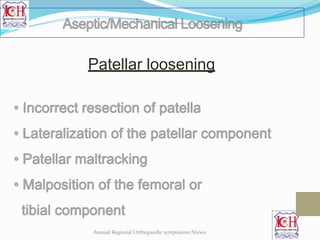
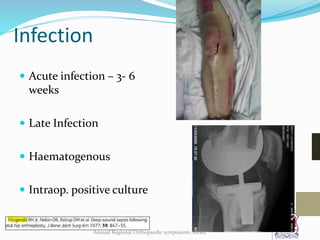
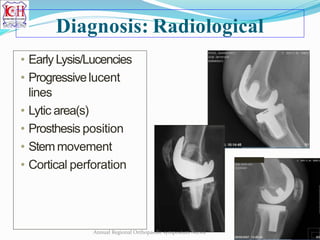
The document discusses total knee replacement (TKR) and defining its failure. An ideal TKR has properly aligned components in the correct anatomical planes with balanced soft tissues. Failure is defined as requiring revision surgery, with the main causes being aseptic loosening, deep infection, and pain. Joint registries provide data on patient characteristics, implants, and surgical techniques to evaluate safety and cost-effectiveness of TKR. Common indications for revision include aseptic loosening, infection, pain, and patellofemoral issues.


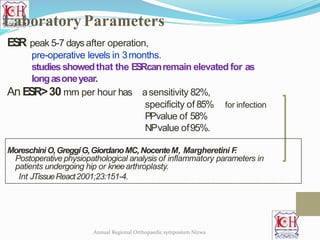
![CRP
level is abetter indicator
early peak 2-3 daysafter surgery,
usually normal - 3 wksafter operation.
CRPvalue>10 mg/l
for infection
96%sensitivity
92%specificity
74%PPV
99%NPV
GreidanusNV,Masri BA,GarbuzDS,et al. Useof erythrocyte sedimentation rate
and C-reactive protein level to diagnose infection before revision total knee
arthroplasty: a prospective evaluation. JBoneJointSurg[Am] 2007;89-A:1409-16.Annual Regional Orthopaedic symposium Nizwa](https://image.slidesharecdn.com/whydototalkneesfail-180224181719/85/Why-do-total-knees-fail-16-320.jpg)
![Interleukin 6 (IL-6)
elevated (> 10 pg/mL )
peri-prosthetic infection, higher predictivevalue
Interleukin-6 levels
peak - first 6 to 12hours
baseline- 48 to 72 hours.
Acombination of CRPandIL-6hasrecentlybeenshown
to provide excellent sensitivityin the assessmentof
infection after TKR.
Bottner F,ErrenM, WegnerA, Winkelmann K,et al.
Interleukin-6, procalcitonin and TNFalpha: markers of peri-
prosthetic infection following total joint replacement. JBoneJoint
Surg[Br] 2007;89-B:94-9.
Annual Regional Orthopaedic symposium Nizwa
Alpha Defensin
Leucocyte esterase](https://image.slidesharecdn.com/whydototalkneesfail-180224181719/85/Why-do-total-knees-fail-17-320.jpg)
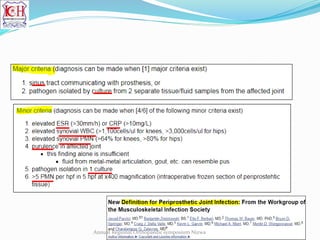


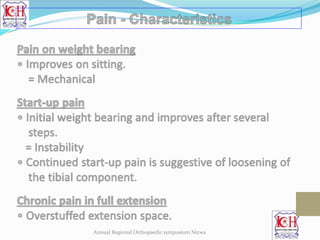
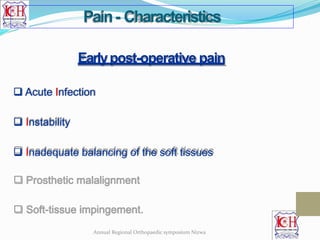
![Ideally the pain should be largelyrelieved
in most of thecases
by 3 months postoperatively.
Bakeret al, JBoneJointSurg [Br]2007;89-B:893-900
Study involving more than 8000 patients reported that 19.8%had
persistent pain one year after operation.
Avisualanaloguescale(VAS)ishelpfulindocumenting.
Pain
Annual Regional Orthopaedic symposium Nizwa](https://image.slidesharecdn.com/whydototalkneesfail-180224181719/85/Why-do-total-knees-fail-21-320.jpg)
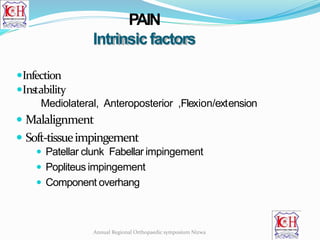

![ Early post-operative period
• Uncorrected pre-operative ligamentous imbalance
• Improper intra-operative ligamentous balancing
• Mismatch of the flexion-extension gap
• Iatrogenic injury to the ligaments during surgery
• Pre-existing neuromuscular pathology
Late instability
• Malalignment leading to progressive stretching of ligaments
• Wear of polyethylene
• Loosening of the component and collapse
Parratte S, Pagnano MW. Instability after total knee arthroplasty. J Bone
JointSurg [Am] 2008;90-A:184-94.Annual Regional Orthopaedic symposium Nizwa](https://image.slidesharecdn.com/whydototalkneesfail-180224181719/85/Why-do-total-knees-fail-34-320.jpg)