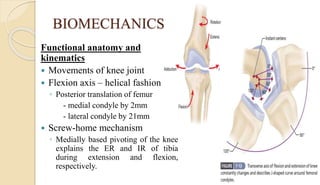
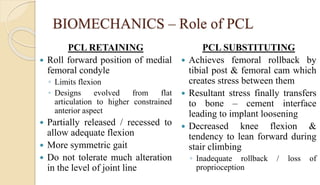
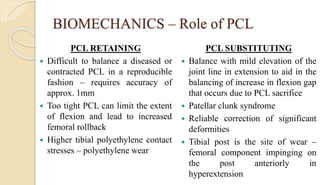
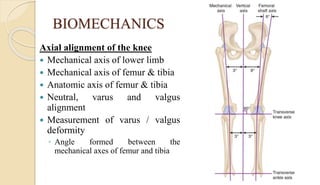
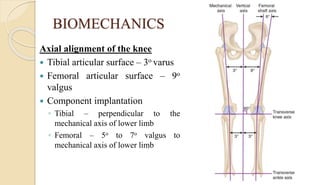
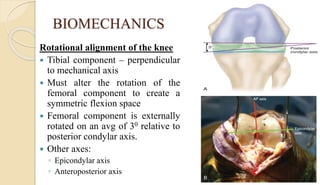
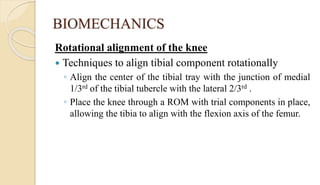
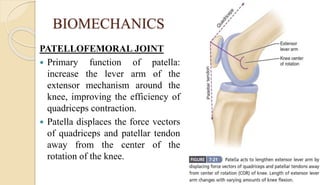
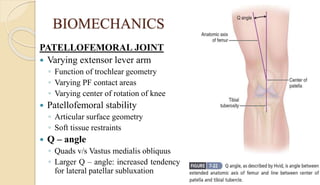
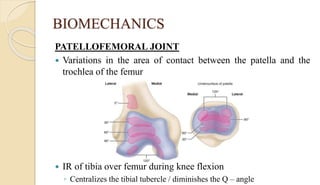
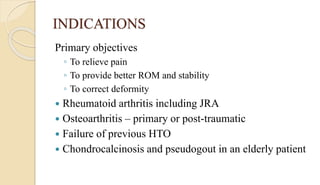
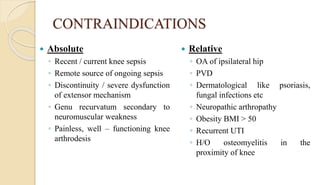
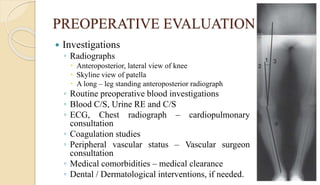
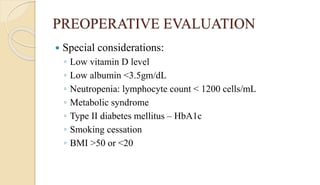
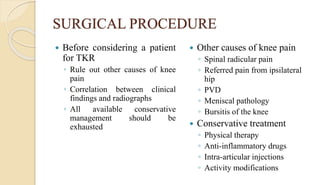
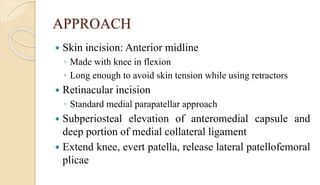
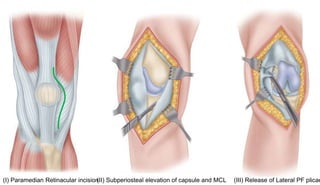
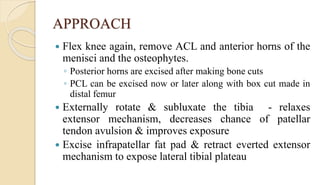
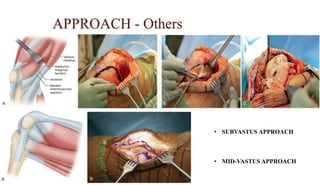
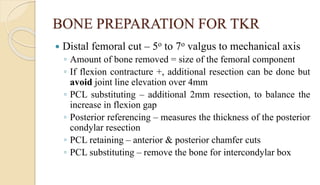
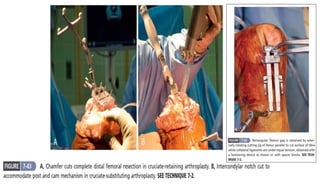
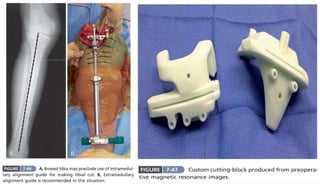
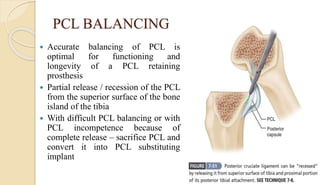
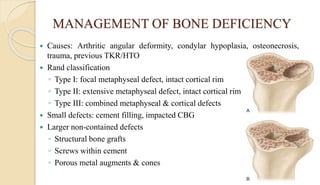
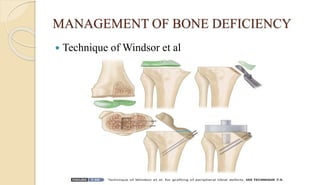
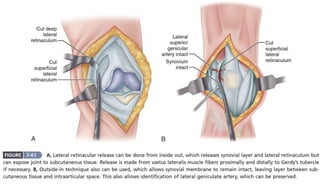
Total knee replacement involves replacing the knee joint with prosthetic components. Critical elements for success include proper anatomy, biomechanics, soft tissue balancing and alignment. A thorough preoperative evaluation is important. The surgical procedure involves exposing the knee joint through an incision and removing damaged bone and cartilage. Bone cuts are made to prepare the femur and tibia to receive prosthetic components. Proper alignment and soft tissue balancing are crucial. Factors like deformity, bone loss, and patellofemoral tracking must be addressed. Attention to surgical technique and postoperative rehabilitation can provide pain relief and improved function.