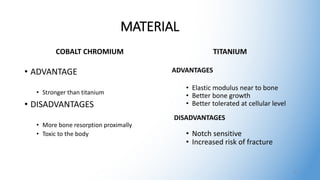
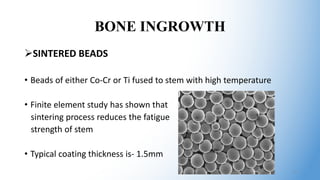
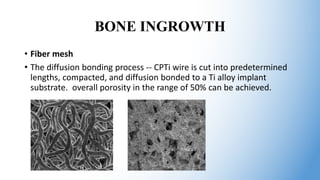
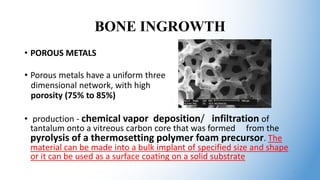
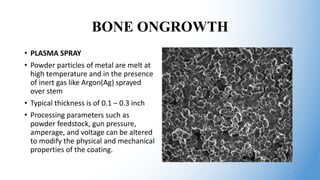
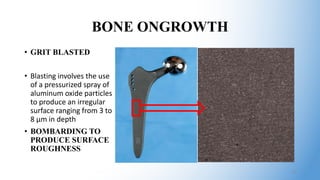
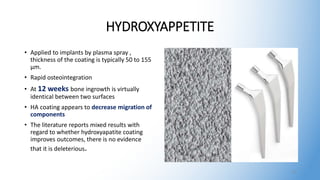
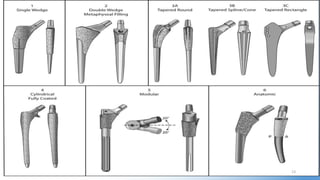
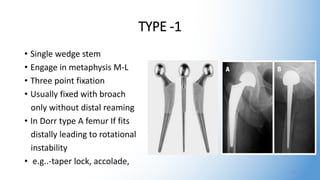
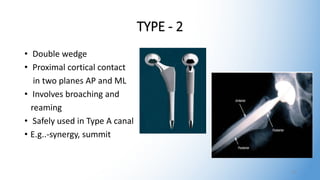
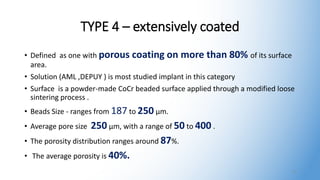
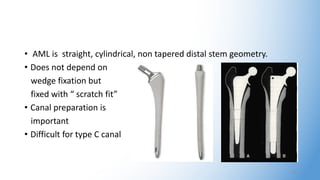
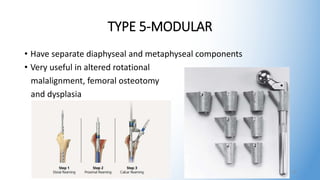
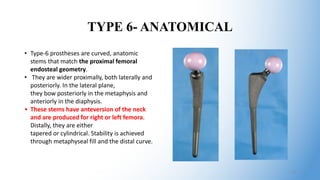
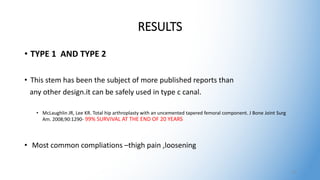
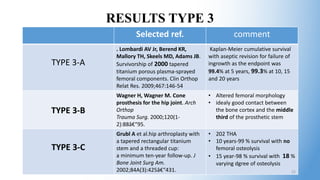
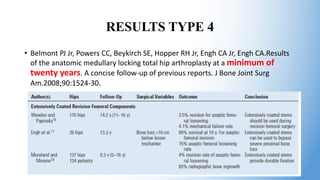
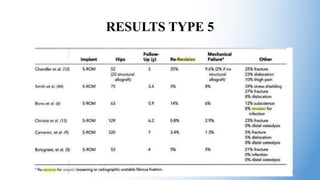
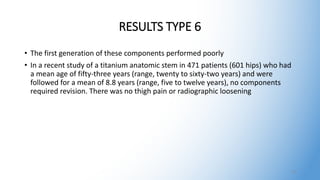
The document discusses uncemented femoral components in orthopedic surgery, highlighting material options such as cobalt chromium and titanium along with their respective advantages and disadvantages. It covers important aspects of bone ingrowth and ongrowth, various stem designs, and presents survival rates and results from different implant types, emphasizing the long-term efficacy of cementless fixation. The conclusion advocates for the appropriate use of cementless femoral designs, noting their potential benefits for both young and older patients.