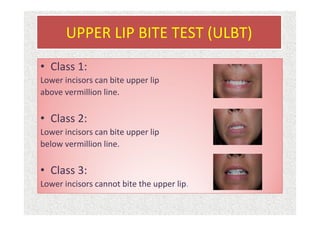
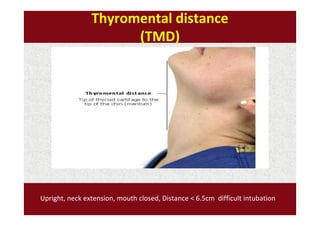
The document discusses guidelines for pre-anesthetic evaluation. It outlines the objectives of pre-anesthetic evaluation as assessing the patient's medical condition, optimizing risks for anesthesia, and obtaining informed consent. Key components of evaluation include medical history, physical exam assessing airway and cardiovascular/respiratory systems, lab tests, and ASA physical status classification. Guidelines are provided for pre-op fasting, medication management, documentation, and conducting evaluations via interview or questionnaires.