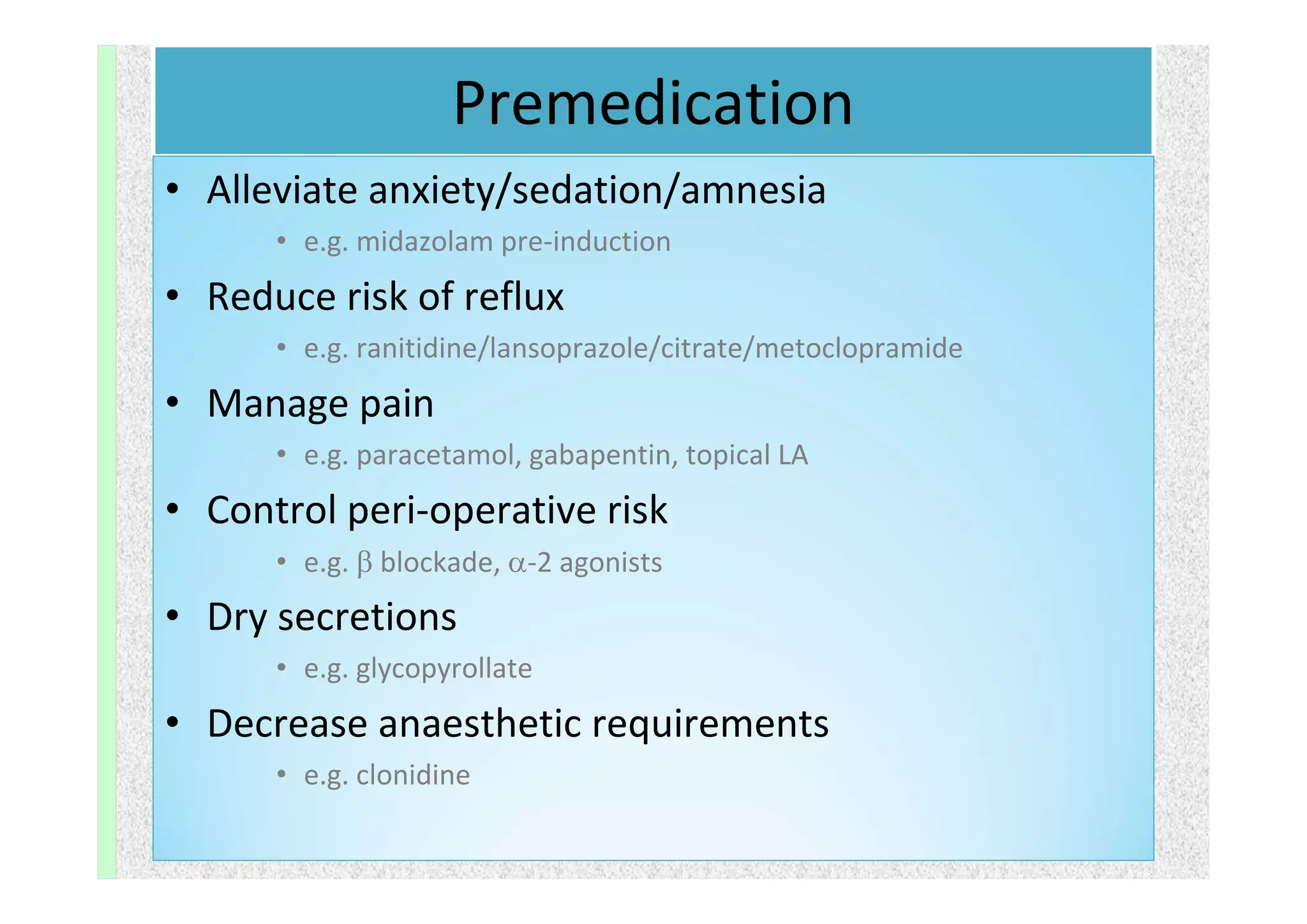
The document outlines the essential components of pre-anesthetic evaluation, emphasizing the anaesthesiologist's role in assessing and optimizing patient conditions to minimize risks during surgery. It details the evaluation process, including medical history, physical examinations, and necessary investigations to identify potential complications. Overall, an effective pre-anesthetic assessment can reduce healthcare costs, patient anxiety, and enhance the safety and quality of perioperative care.