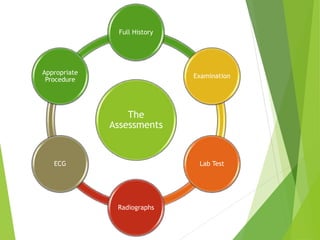
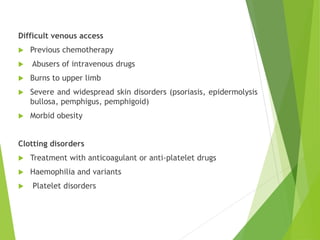
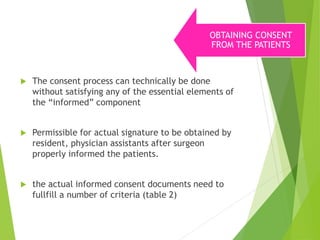
This document discusses pre-operative assessment and preparation of surgical patients. It outlines the goals of pre-operative evaluation which include identifying medical issues, determining if further information is needed, and ensuring the patient is medically optimized for surgery. It also discusses informed consent, appropriate pre-operative tests and investigations, prophylactic measures to prevent complications, anesthesia considerations, and assessing post-operative intensive care needs.