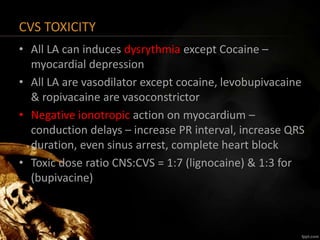
Local anesthetics work by blocking sodium channels and interrupting nerve conduction. They are classified based on their chemical structure as esters or amides. Amides like lidocaine and bupivacaine are metabolized in the liver and have a lower risk of allergic reactions compared to esters. The potency, onset, and duration of local anesthetics depends on factors like lipid solubility, dose, pH, and addition of vasoconstrictors. Toxicity from local anesthetics is related to the dose administered and rate of absorption. Early symptoms of toxicity involve the central nervous system like agitation and seizures. Later, cardiovascular symptoms like arrhythmias and hypotension can occur. Treatment involves stopping administration, managing