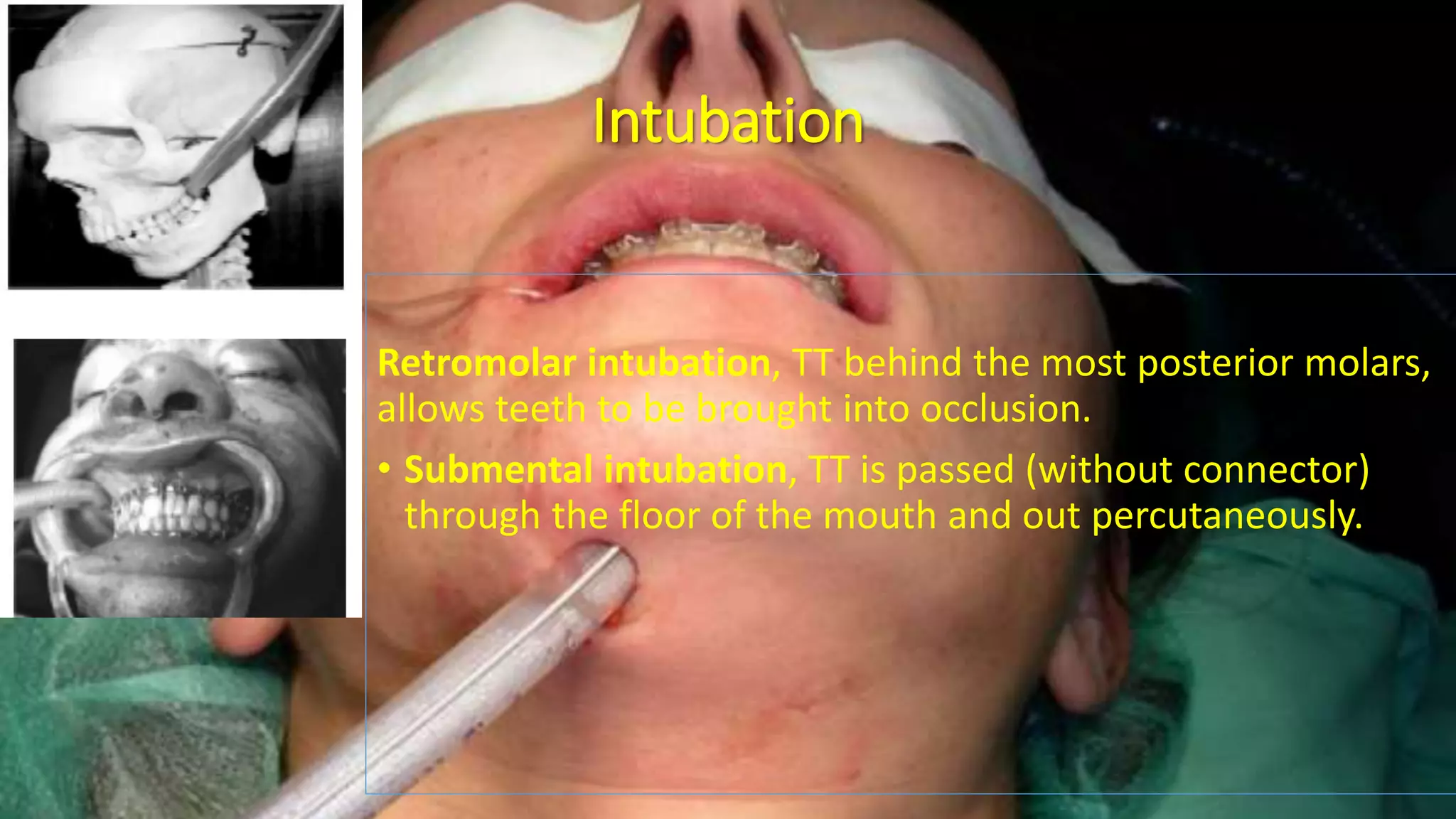
Maxillofacial surgery involves the head, neck, face and jaws and can be done for congenital deformities, injuries, or tumors. Anesthesia for these procedures presents several challenges including a shared airway, potential for difficult intubation, blood loss requiring induced hypotension, and risks during emergence like airway obstruction. Careful pre-operative planning is important to choose the best airway management strategy and prevent complications. Induced hypotension can improve surgical conditions but risks need to be weighed. Emergence and extubation also require vigilance to address swelling and ensure hemostasis and a secure airway.