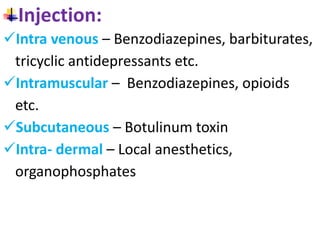
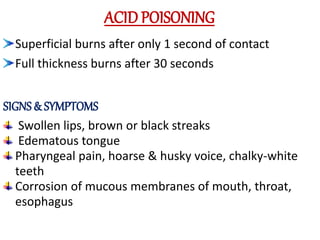
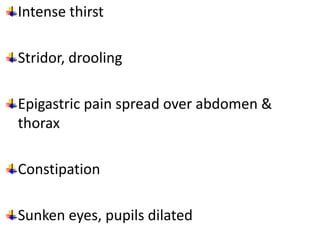
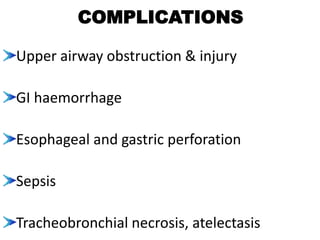
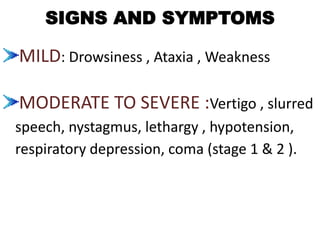
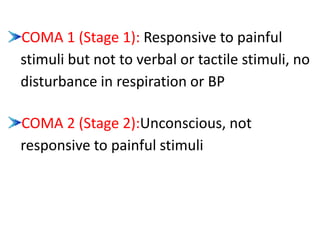
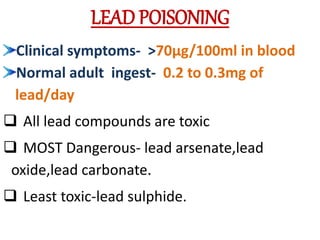
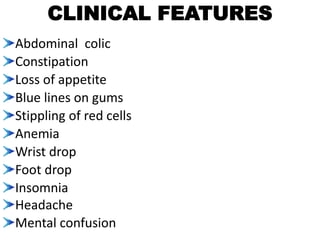
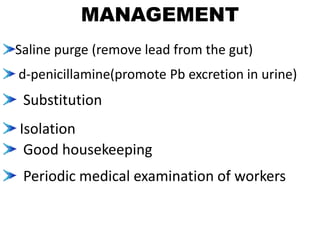
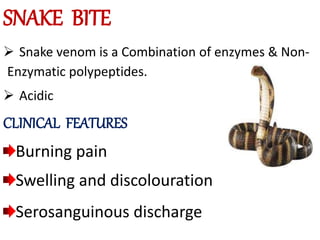
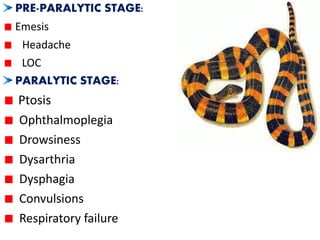
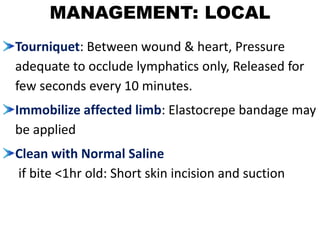
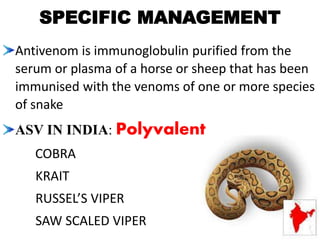
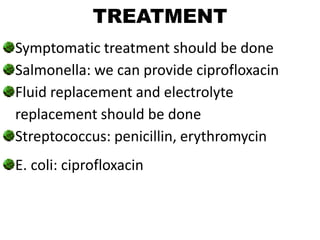
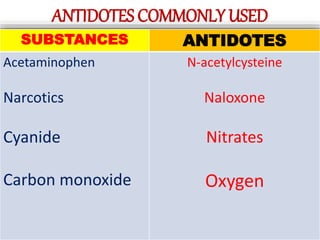
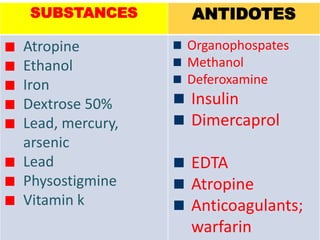
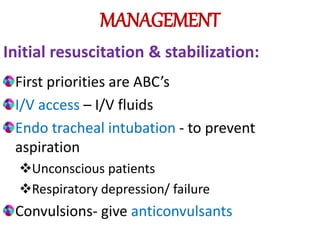
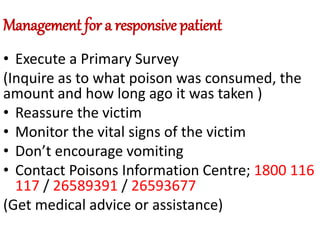
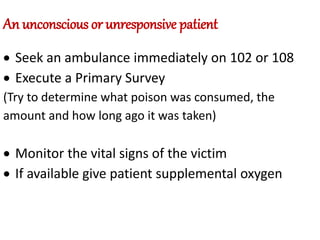
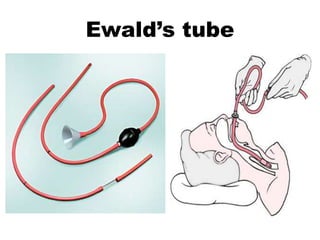
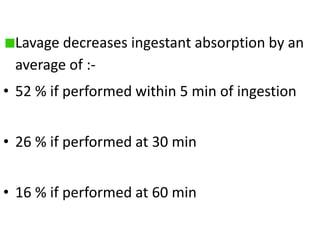
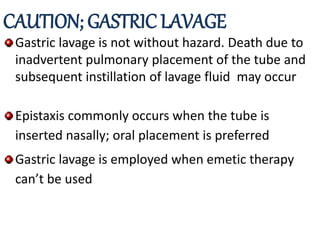
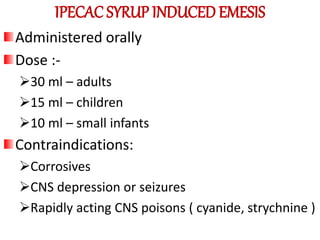
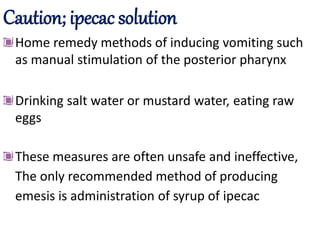
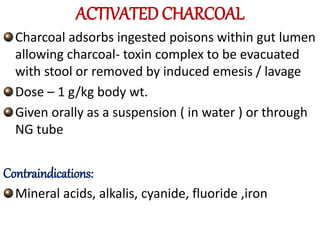
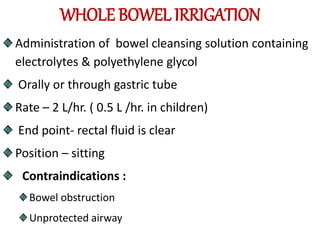
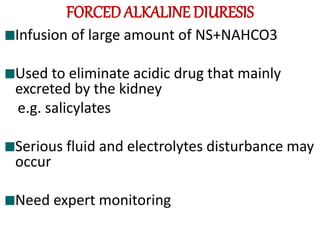
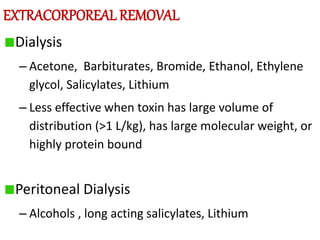
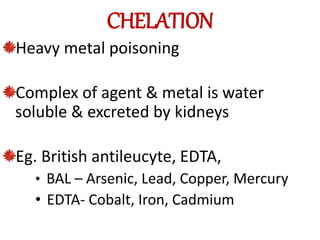
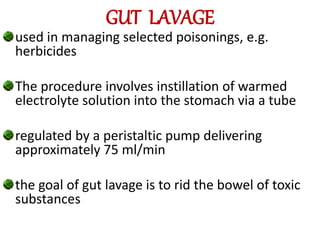
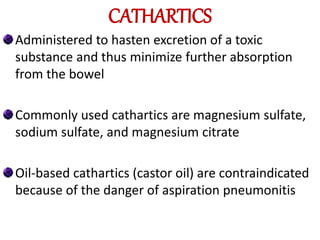
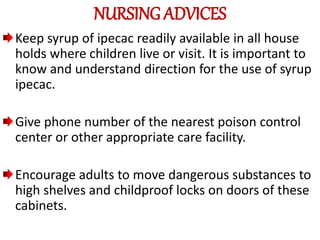
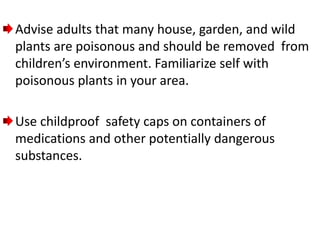
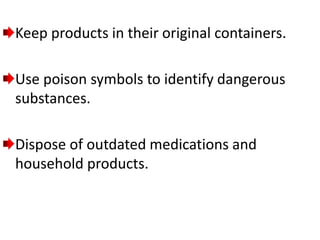
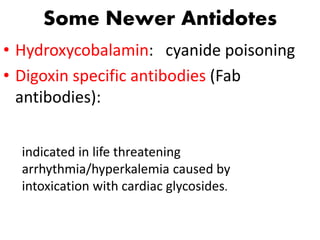
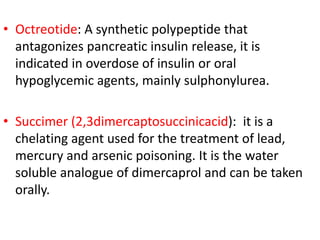
This document discusses various aspects of poisoning management, including classification, routes of poisoning, signs and symptoms of specific poisons like acids, benzodiazepines, lead, and snakes. It also covers management strategies like gastric lavage, ipecac syrup, activated charcoal, whole bowel irrigation, forced alkaline diuresis, and chelation therapy. The goal of management is removal or neutralization of toxins while stabilizing the patient.