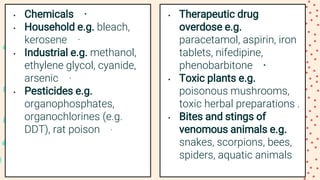
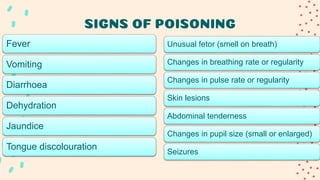
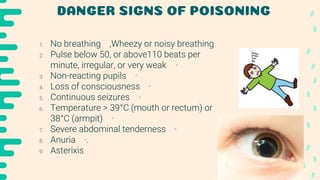
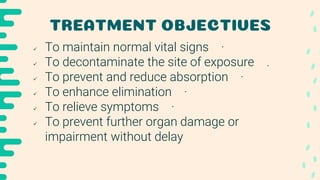
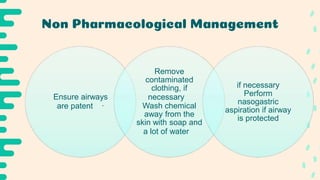
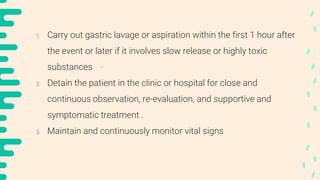
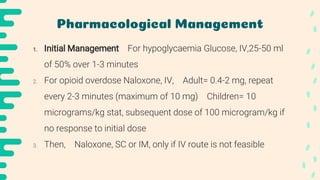
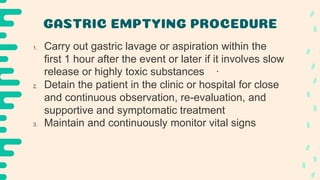
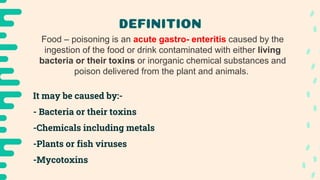
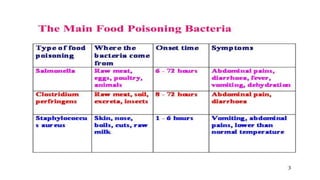
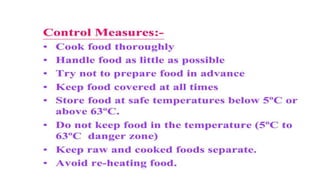
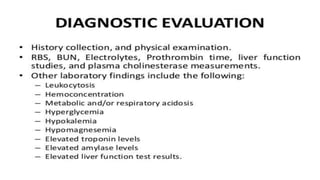
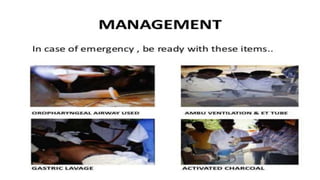
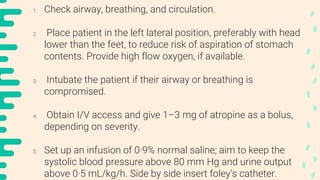
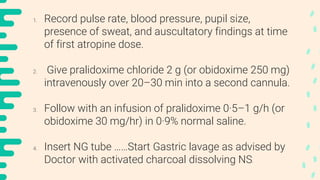
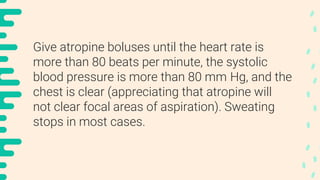
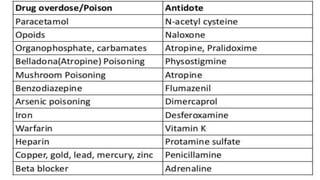
Poisoning represents harmful effects from accidental or intentional exposure to toxic substances. The main types are ingestion, inhalation, injection and absorption. Poisoning may cause local or systemic effects immediately or delayed. Causes include chemicals, household products, pesticides, therapeutic drugs, and toxic plants/animals. Signs include vomiting, diarrhea, difficulty breathing and skin rashes. Danger signs require urgent treatment like lack of breathing. Investigations include toxicology analysis and organ function tests. Treatment aims to maintain vital signs, decontaminate, enhance elimination and relieve symptoms. Management depends on specific poison but may include decontamination procedures, antidotes and supportive care.