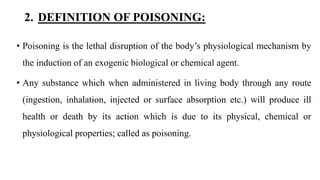
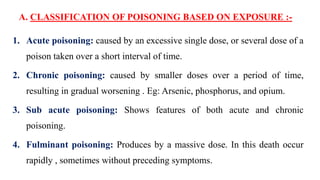
The document discusses poisoning and drug overdose management. It defines poisoning, classifies different types of poisons and poisoning, and describes common causes and clinical manifestations of poisoning. It then provides more detailed information about organophosphorus poisoning and lead poisoning, including sources, pathophysiology, signs and symptoms, diagnosis, and management. The goal of treatment is to reduce absorption, enhance elimination, and neutralize toxins. Organophosphorus poisoning requires atropinization to counteract excess acetylcholine. Lead poisoning inhibits hemoglobin and enzyme production.














![ SOURCES OF ORGANOPHOSPHATES :-
• Insecticides - malathion, parathion, ethion, diazinon
• Nerve gases - (sarin, woman, tabun – German military used it for
warfare), VX(invented by the English for warfare)
• ophthalmic agents - echothiophate, isoflurophate
• Herbicides - tributes [DEF], merphos](https://image.slidesharecdn.com/poisoning-200509045634/85/Poisoning-18-320.jpg)