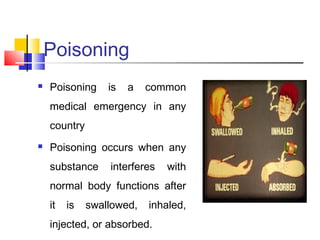
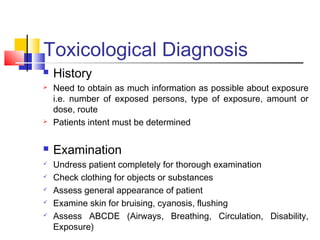
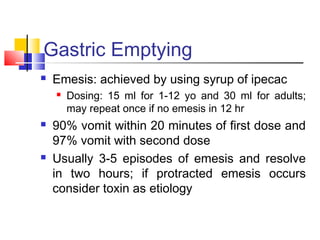
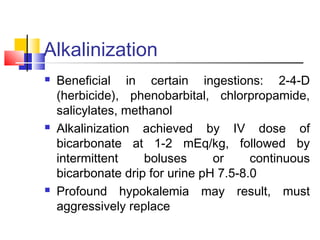
This document discusses poisoning, its causes, symptoms, and management. It defines poisoning as occurring when a substance interferes with normal body functions after being swallowed, inhaled, or absorbed. Common causes of poisoning include cleaning products, pesticides, metals, drugs, contaminated food, and plant toxins. Symptoms vary depending on the poison but can include vomiting, diarrhea, nausea, rash, confusion, and trouble breathing. Management involves resuscitation, diagnosis, decontamination through gastric emptying or charcoal, enhanced elimination such as forced diuresis or dialysis, and administration of antidotes as needed. Prevention strategies include proper storage and disposal of medications and household chemicals.