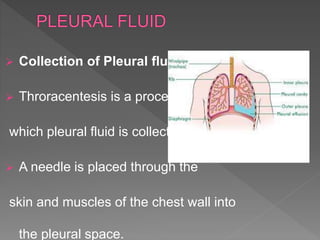
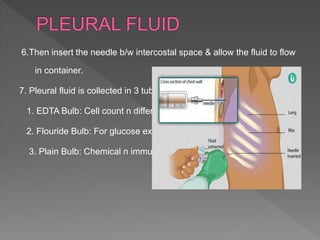
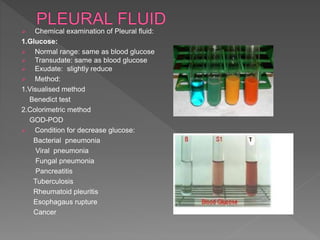
The document provides a detailed overview of pleural fluid, its function, collection, and examination methods. It highlights the formation, composition, and the various conditions leading to pleural fluid accumulation, including infections and neoplasms. Additionally, it outlines the procedures for fluid collection and the subsequent physical, chemical, and microscopic examinations to analyze pleural fluid samples.