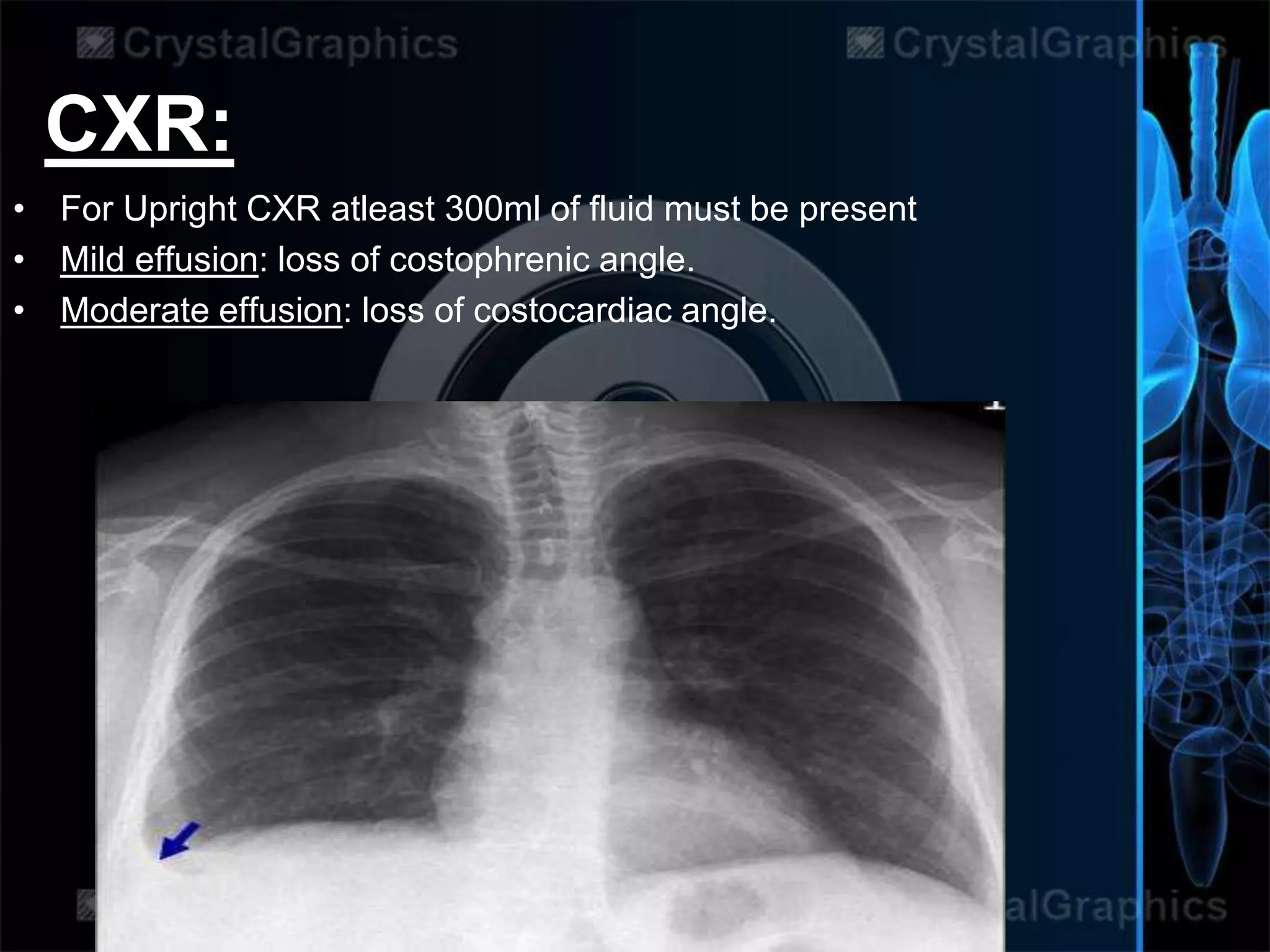
This document provides information about pleural effusions. It defines a pleural effusion as excess fluid buildup between the pleural layers outside the lungs. Normally a small amount of fluid is present and circulated, but over 25mL is considered an effusion. Effusions are classified as transudative or exudative based on their characteristics. Symptoms include chest pain and breathing difficulties. Diagnosis involves physical exam, imaging like x-rays, and fluid analysis. Management depends on the underlying cause but may include drainage, medication, or surgery in severe cases.





![TRANSUDATE EXUDATE
Main causes
↑ hydrostatic
pressure,
↓ colloid
osmotic pressure
Inflammation-
Increased vascular
permeability
Appearance Clear Cloudy
Specific gravity < 1.012 >1.020
Protein content < 2.5 g/dL > 2.9 g/dL
Fluid protein/
serum protein(Ratio)
< 0.5 > 0.5
SAAG = Serum
[albumin] - Effusion
[albumin]
> 1.2 g/dL < 1.2 g/dL
Fluid LDH
upper limit for serum
< 0.6 or < 2⁄3
0.6 or > 2⁄3
Cholesterol content < 45 mg/dL > 45 mg/dL](https://image.slidesharecdn.com/pleuraleffusion-180429063711/75/Pleural-effusion-6-2048.jpg)