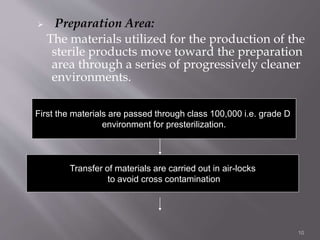
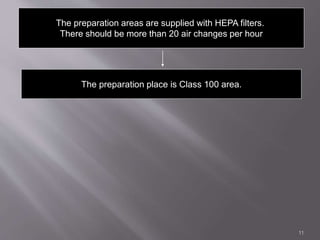
The document discusses the scale-up process of parenteral formulations from the laboratory scale to full production. It explains that the pilot plant acts as an intermediate stage, where the formulation process is tested on a larger scale than the laboratory to work out any issues. This allows the process to be reliably transferred to full production scale. The document also describes the facilities, equipment, and controls needed for sterile production of parenterals, including cleanroom classifications and airflow, process steps, sterilization methods, and quality testing.