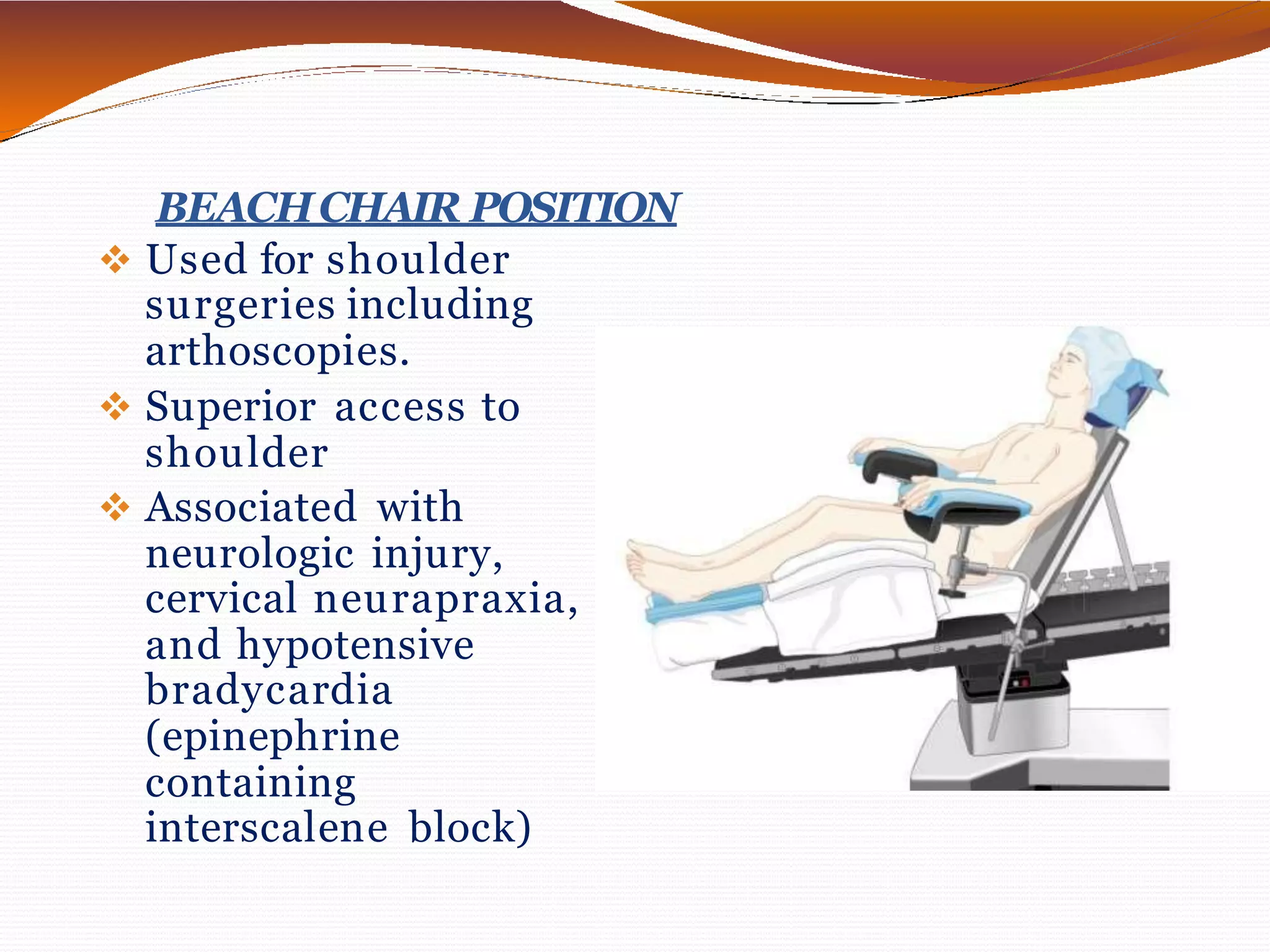
This document discusses various surgical body positions and their physiological effects. It covers positions like supine, Trendelenburg, lithotomy, lateral, and prone. For each position, it describes how it affects cardiovascular, pulmonary and neurological function. Complications are also outlined such as pressure injuries, nerve palsies, and changes in ventilation and oxygenation. Patient positioning is important to balance optimal surgical exposure while preventing physiological harm.