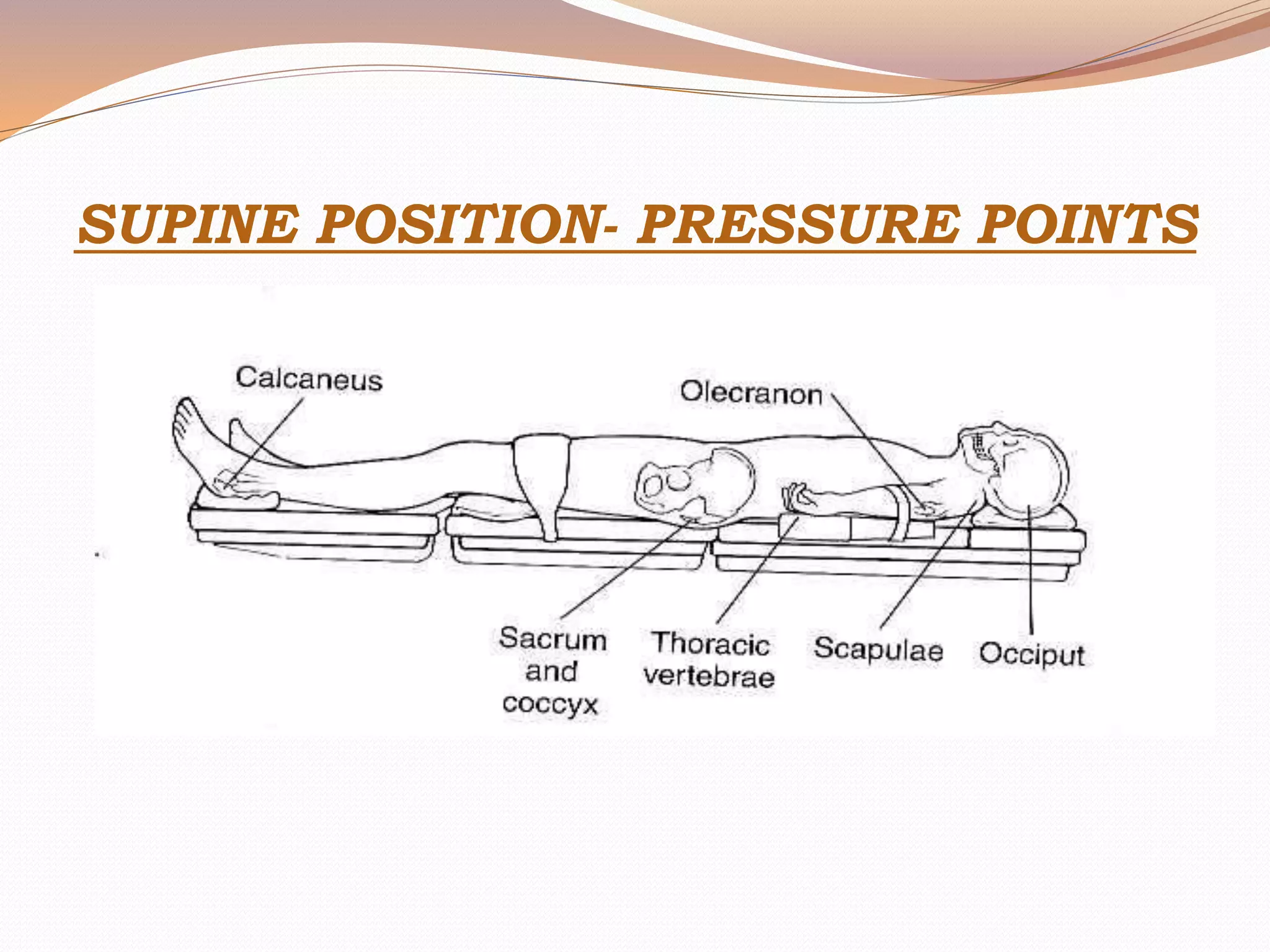
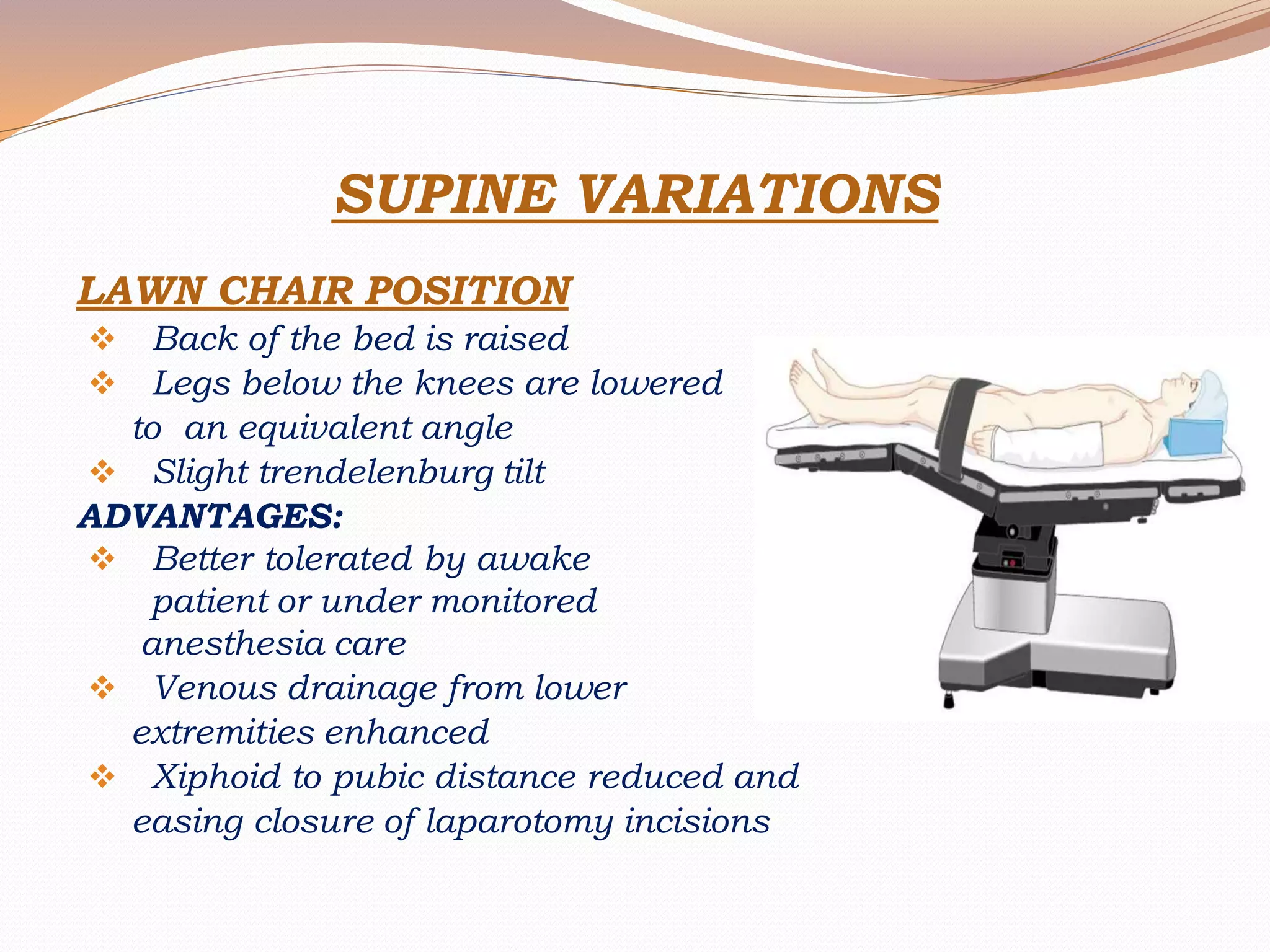
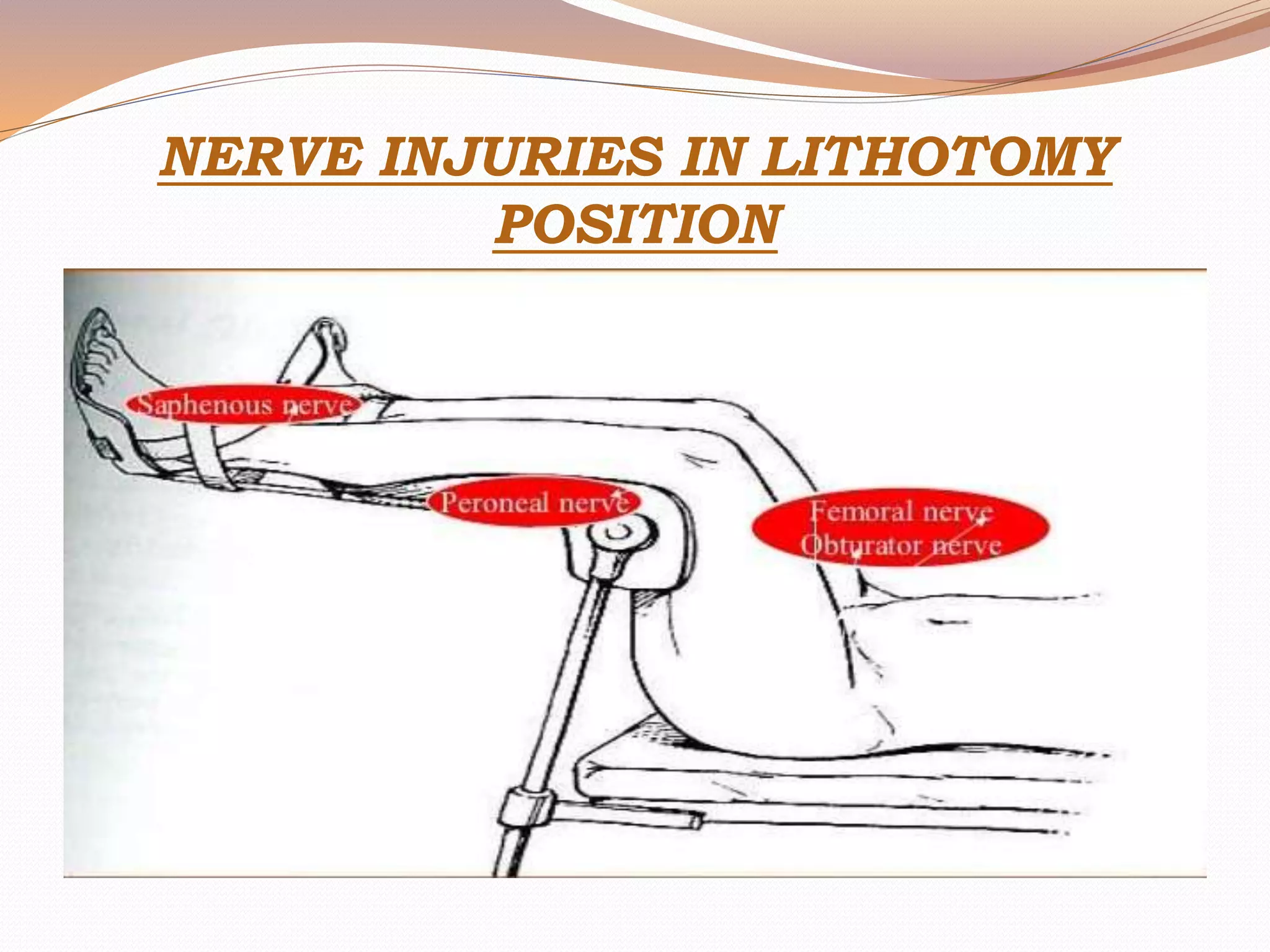
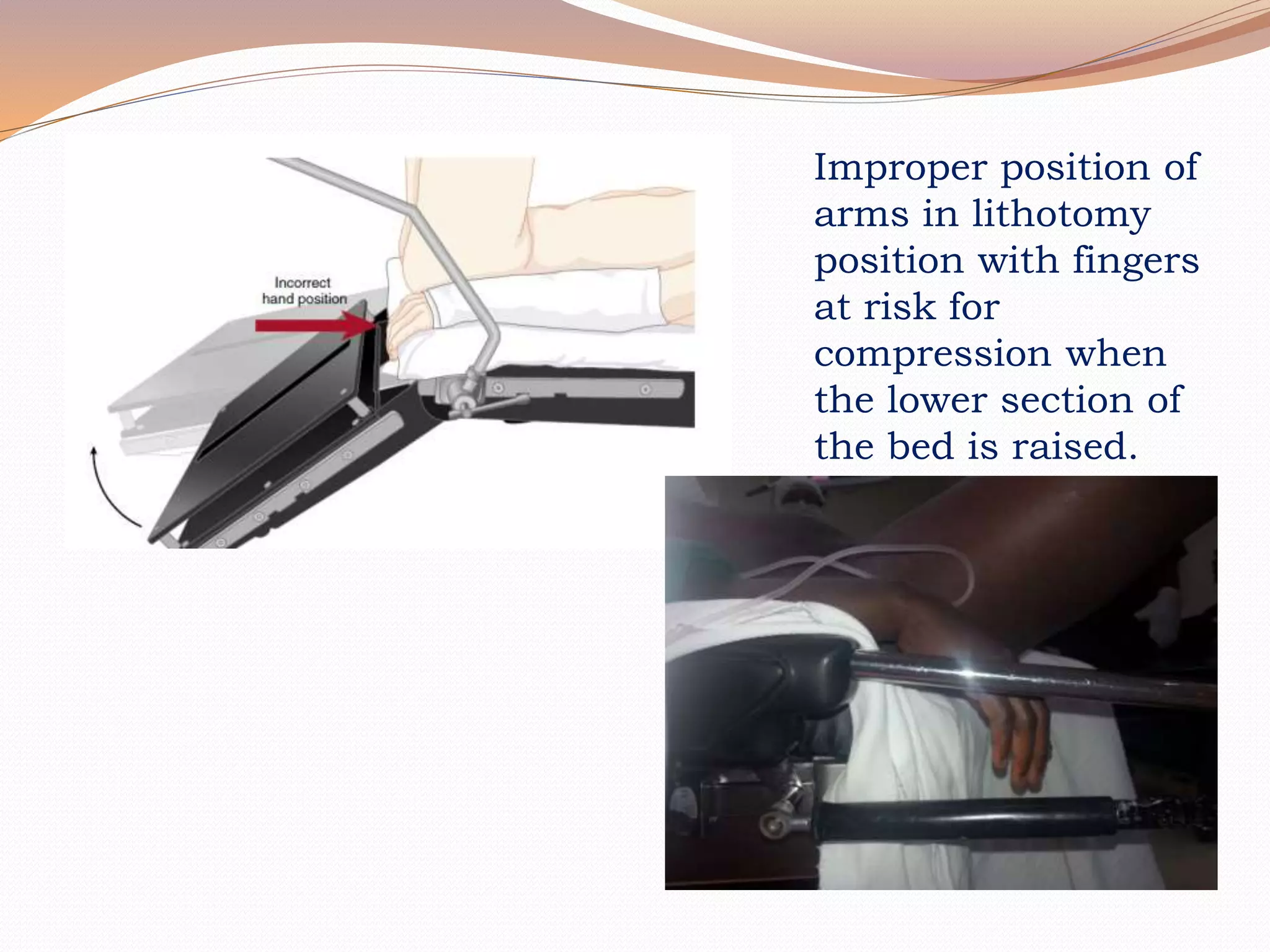
This document discusses various surgical body positions and their physiological effects. It describes positions like supine, lithotomy, lateral, and prone. For each position, it details how positioning impacts cardiovascular and pulmonary function, as well as nerves that may be at risk of injury. Complications from prolonged use of each position are also reviewed. The document emphasizes the importance of careful patient positioning to balance surgical access needs with physiological stability and risk of pressure injuries.