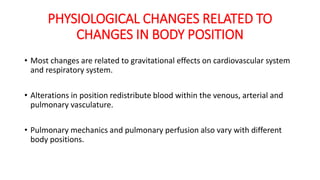
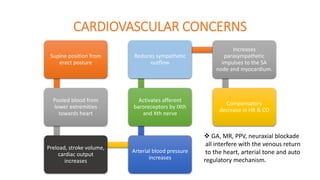
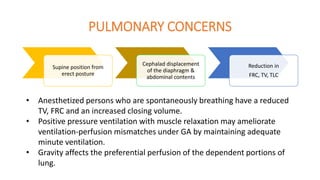
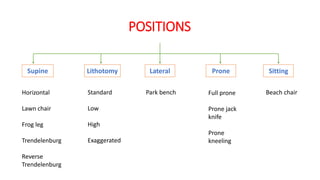
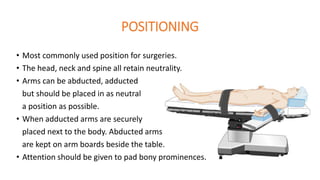
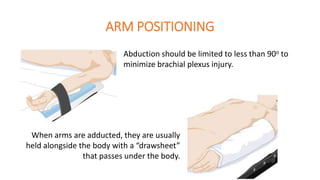
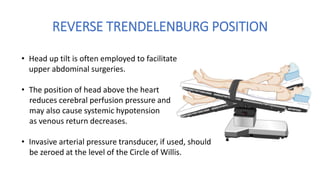
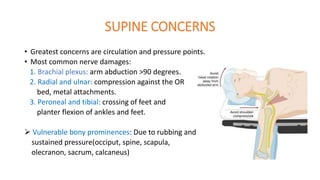
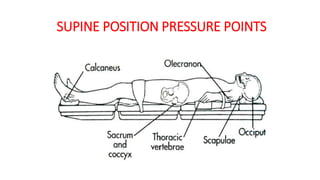
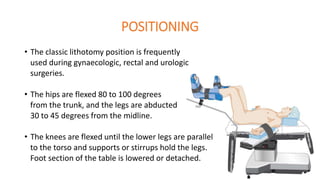
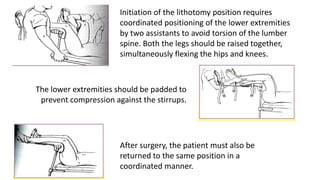
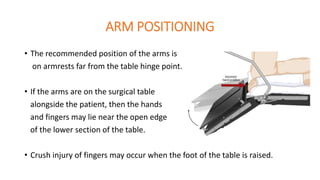
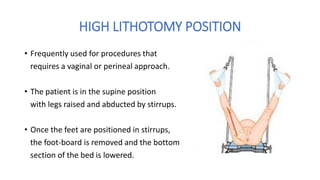
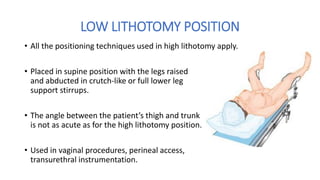
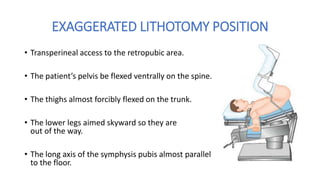
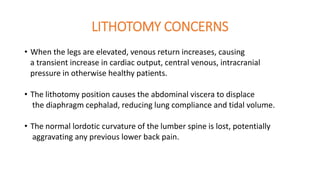
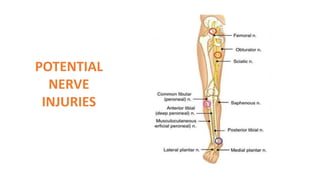
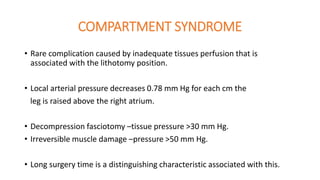
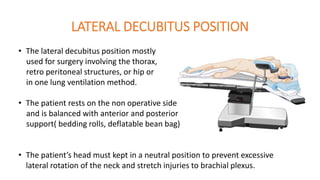
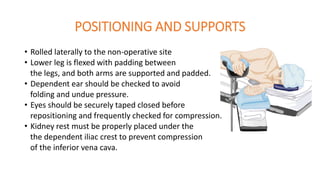
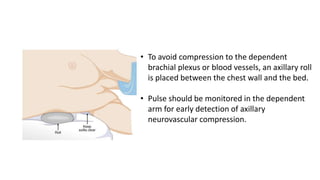
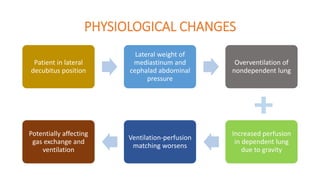
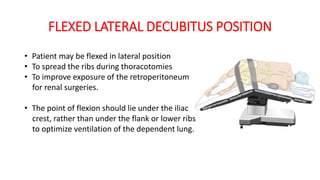
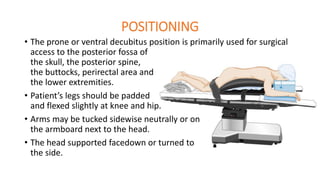
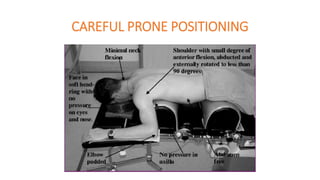
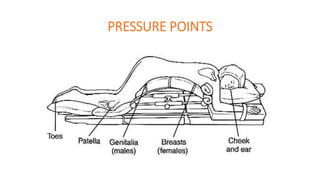
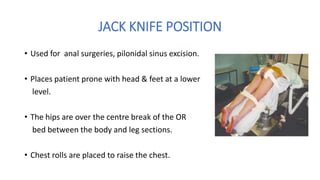
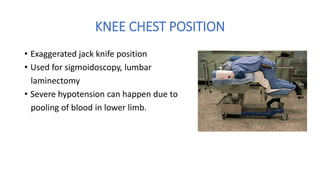
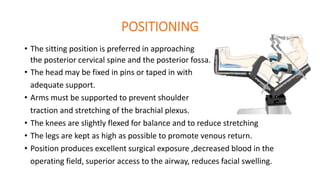
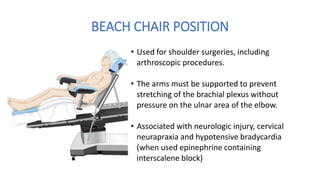
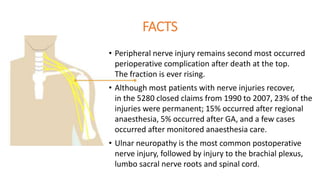
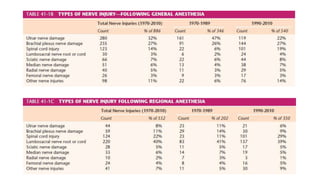
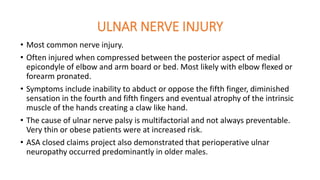
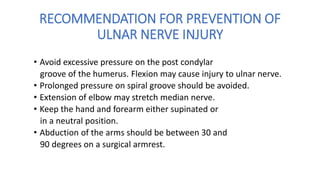
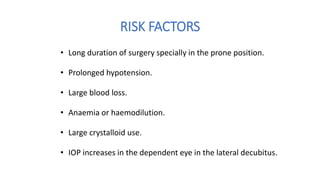
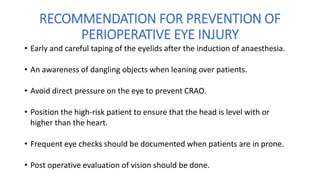
The document discusses the importance of patient positioning in anaesthesia, detailing various surgical positions, their physiological impacts, and potential complications. It emphasizes the need for careful assessment of factors such as surgery duration, patient anatomy, and risk factors to ensure optimal positioning. Additionally, it highlights the associated risks of nerve injury and complications related to each position, underlining the responsibility of the entire surgical team in maintaining patient safety and comfort.