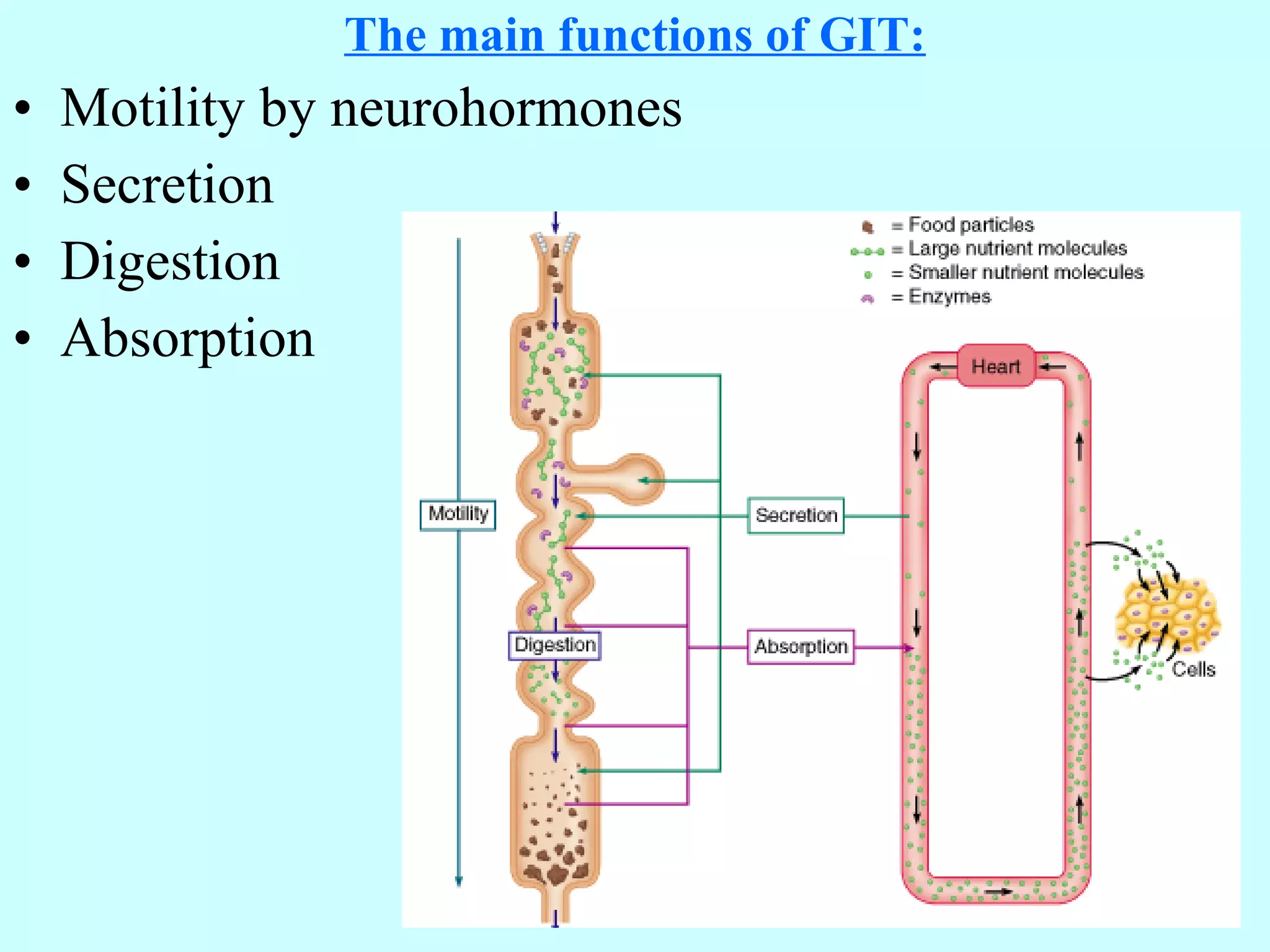
The document summarizes key aspects of gastrointestinal physiology, including:
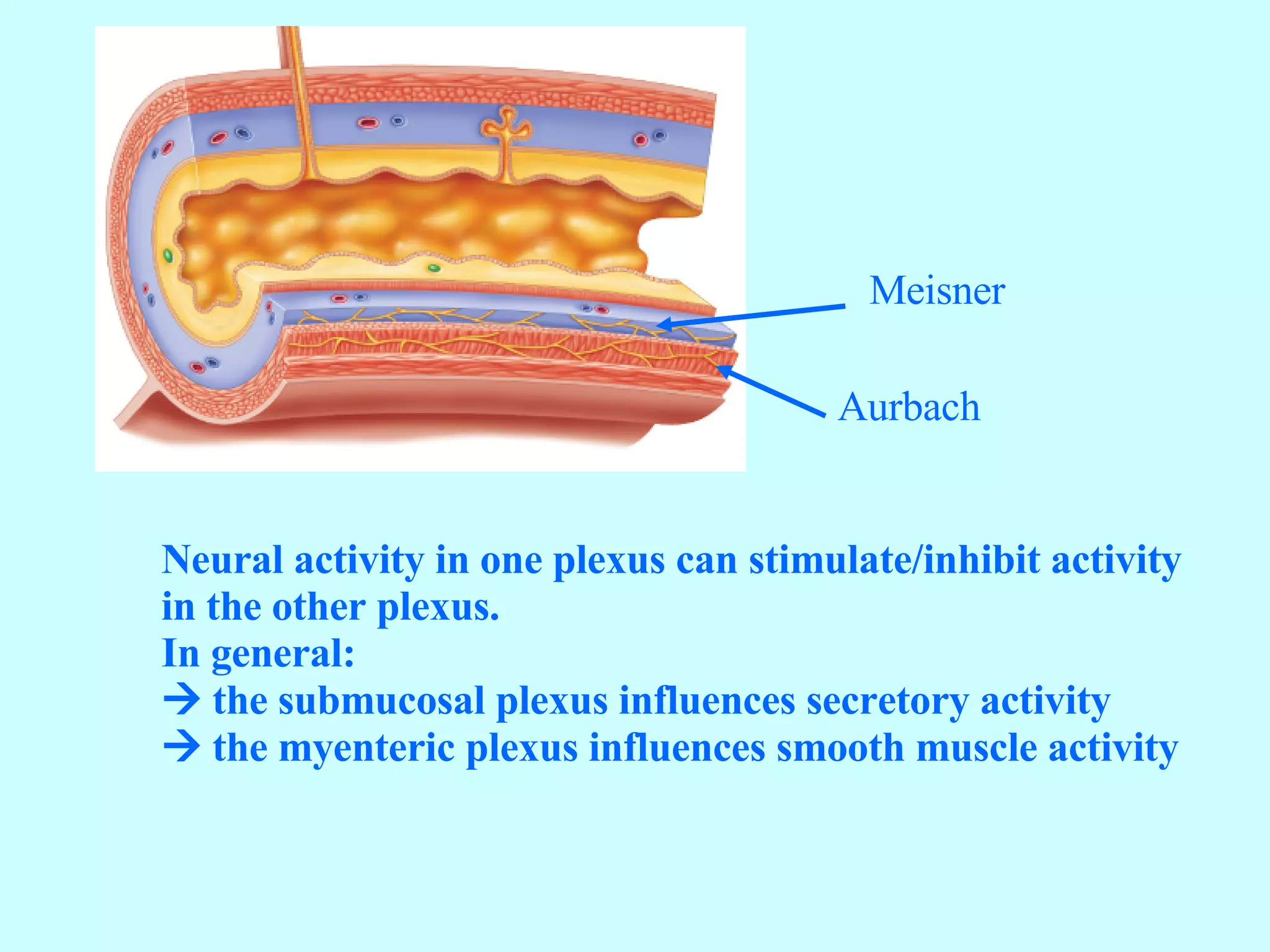
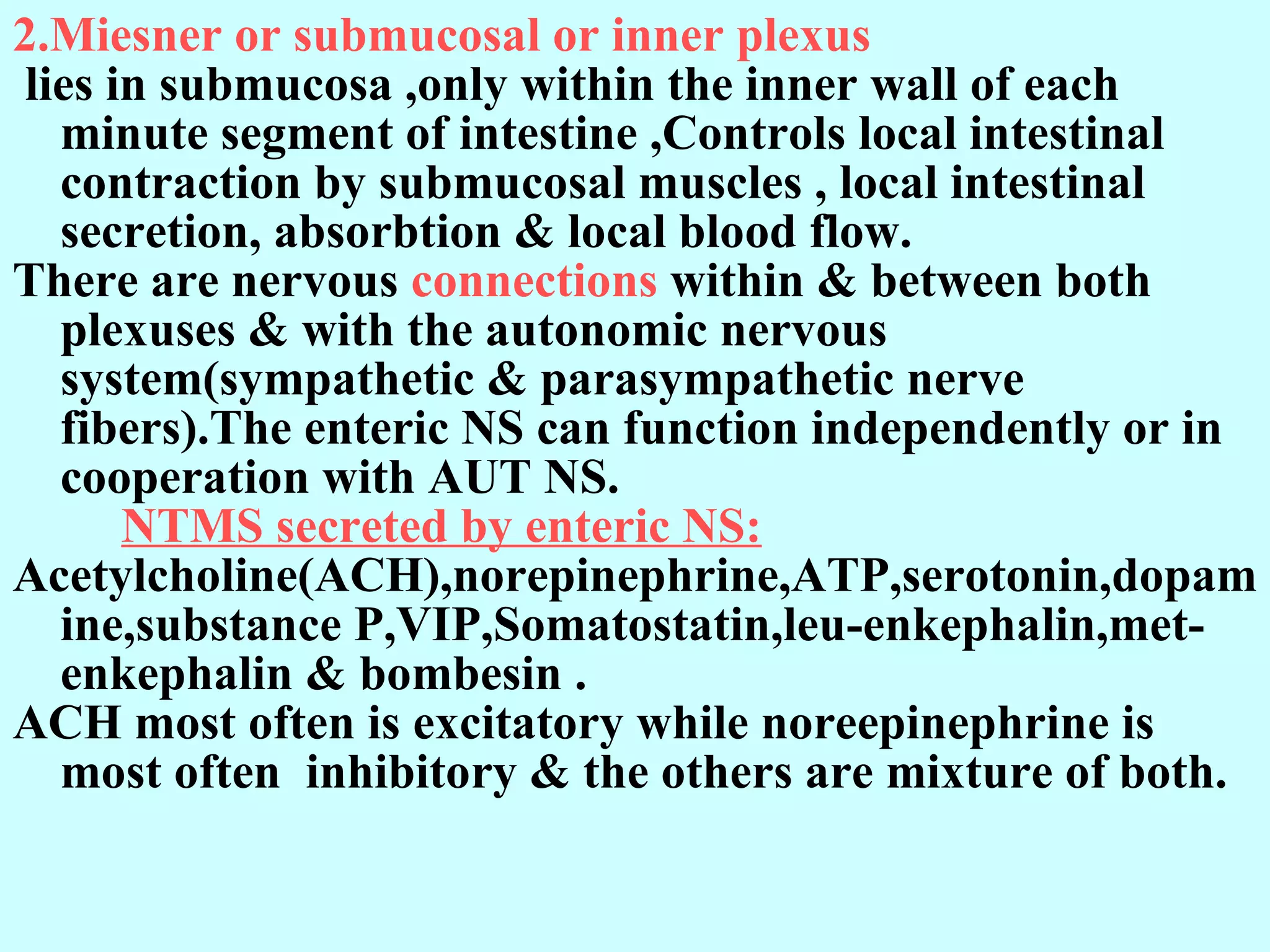
1. The gastrointestinal tract has five layers and contains two nerve plexuses that regulate movement and secretion.
2. Motility in the GI tract involves slow waves and spike potentials mediated by neurotransmitters and hormones.
3. The enteric nervous system and autonomic nervous system control GI motility through parasympathetic and sympathetic fibers.
4. Functional movements include peristalsis for propulsion and segmentation for mixing.
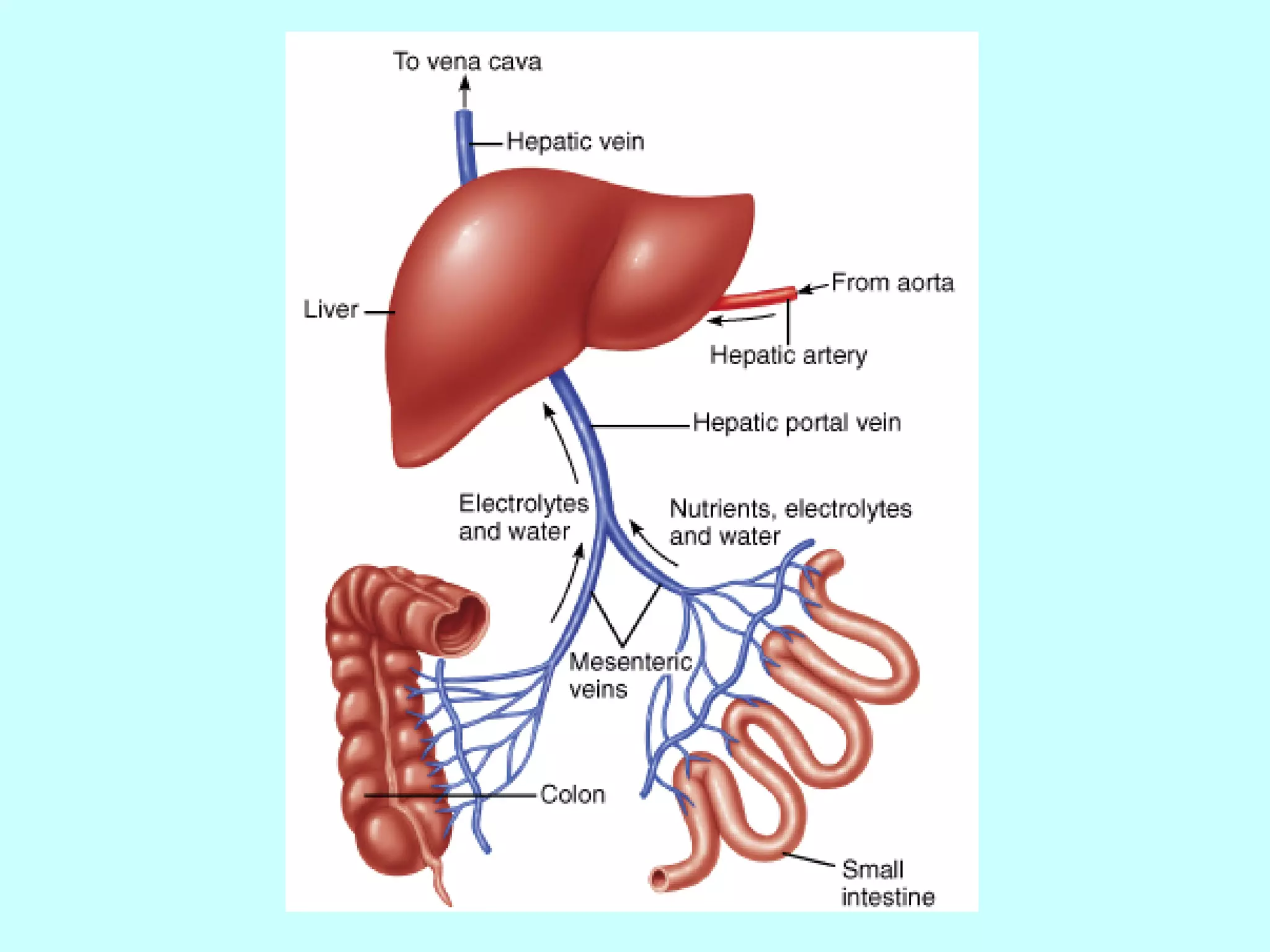
5. Blood flow to the GI tract occurs through several arteries in a countercurrent exchange that optimizes absorption.