This document provides an overview of inflammatory bowel disease (IBD), including ulcerative colitis and Crohn's disease. It discusses risk factors, clinical manifestations, diagnostic testing, and treatment approaches. The main points are:
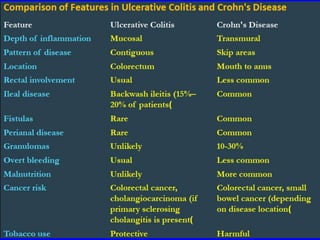
- IBD is characterized by idiopathic inflammation of the gastrointestinal tract. The two main types are ulcerative colitis and Crohn's disease.
- Genetic and environmental factors contribute to risk. Smoking increases risk for Crohn's but decreases risk for ulcerative colitis.
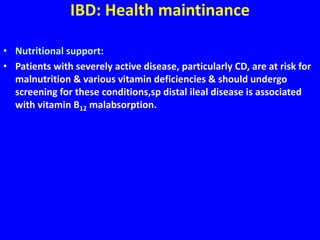
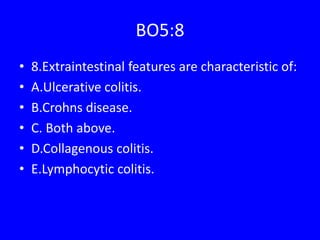
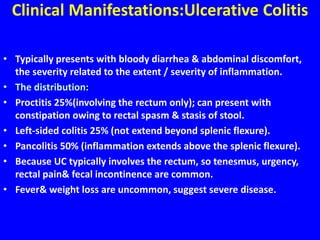
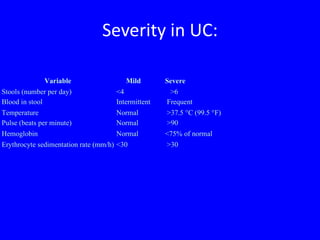
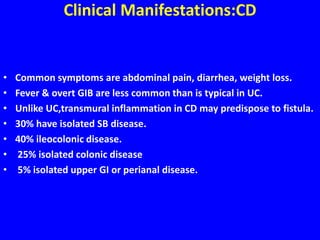
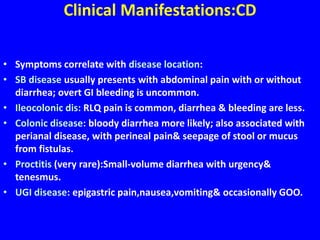
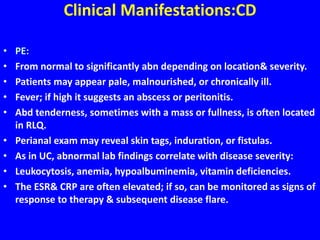
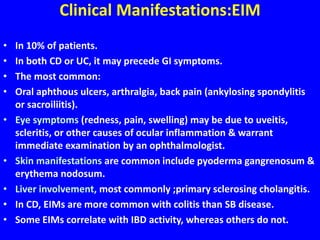
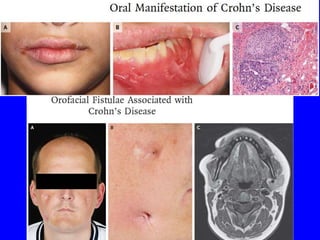
- Symptoms vary based on disease location but may include abdominal pain, diarrhea, bleeding, weight loss, and nutritional deficiencies. Extraintestinal manifestations are more common with Crohn's.




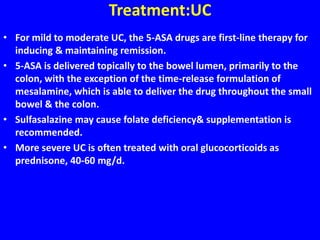
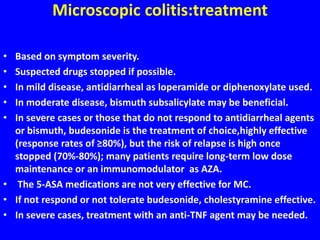
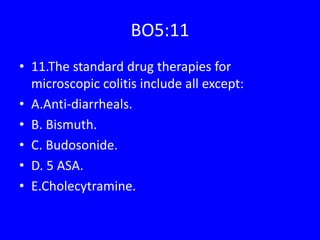
![Treatment:
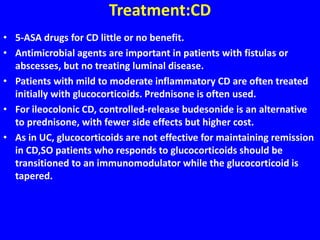
• Budesonide is a glucocorticoid with high first-pass metabolism
available in a controlled ileal-release formulation frequently used in
CD, but (multi-matrix [MMX] system) formulation provides release
of the drug throughout the colon useful in treating UC.
• It has similar efficacy as prednisone but has fewer side effects but
high cost.
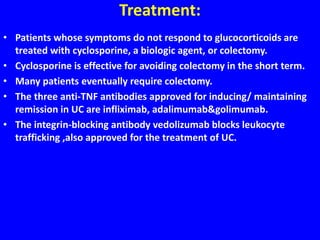
• Patients whose disease does not respond to oral glucocorticoids
should be hospitalized&given IV glucocorticoids or biologic agent.
• Glucocorticoids are not effective for maintaining remission in UC.
• In patients whose disease responds to glucocorticoids, the dose
should be tapered over 2 - 4 months while transitioning to a
maintenance medication (AZA, 6-MP, or a biologic agent).](https://image.slidesharecdn.com/git4thibd2017-170313182835/85/GIT-4th-ibd-2017-26-320.jpg)