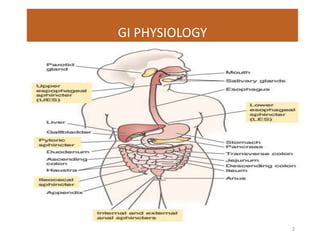
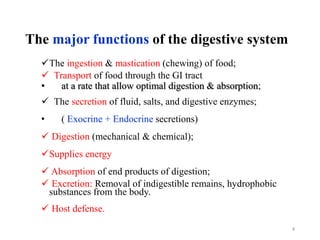
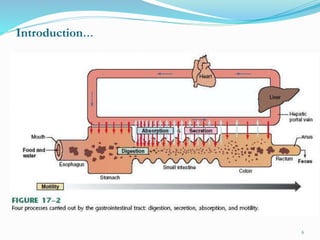
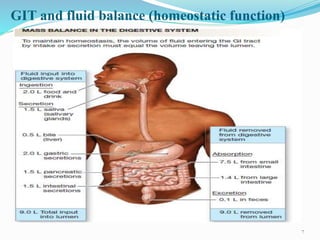
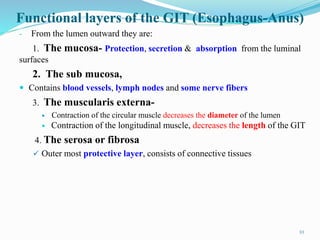
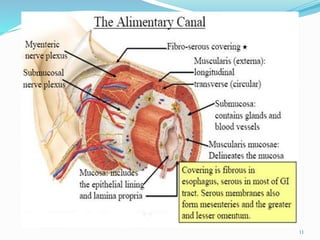
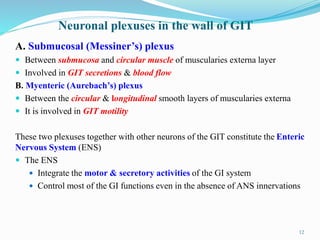
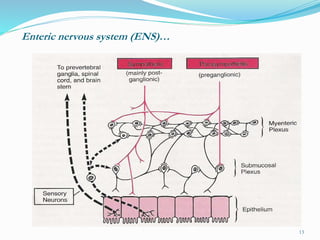
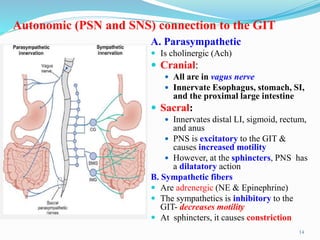
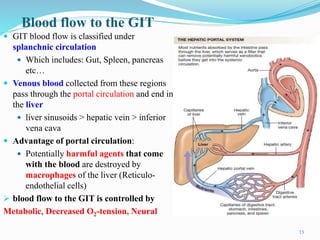
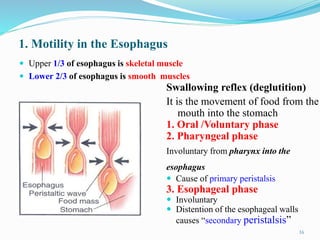
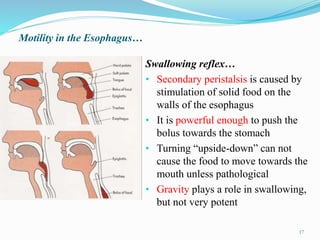
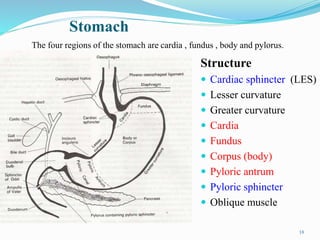
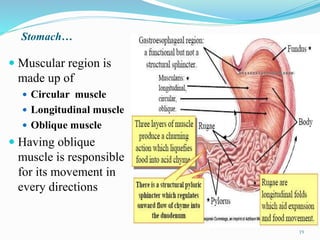
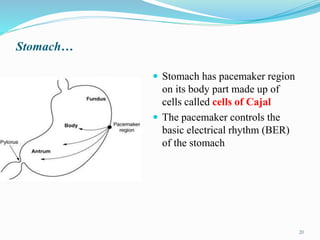
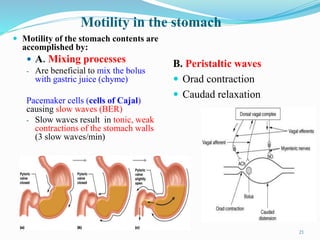
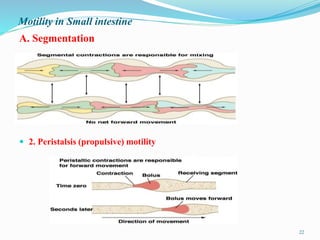
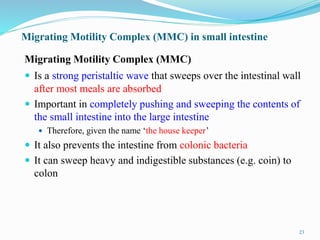
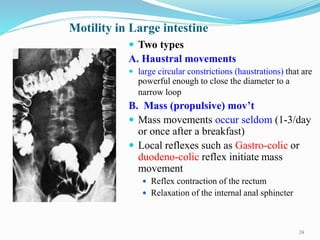
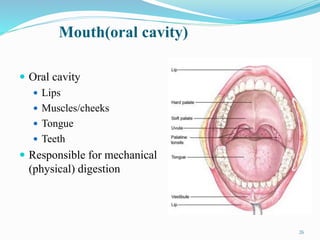
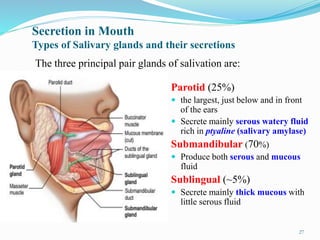
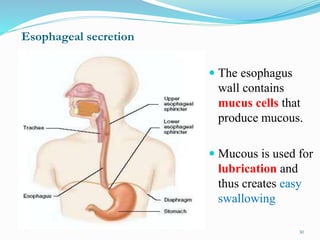
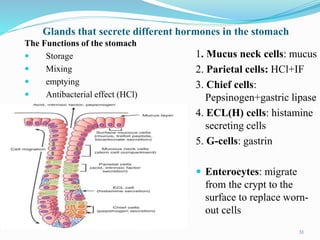
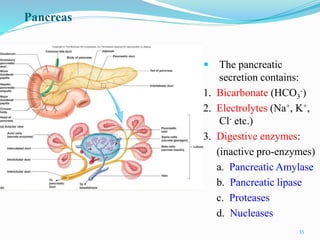
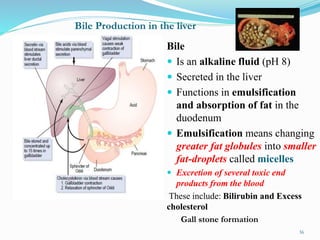
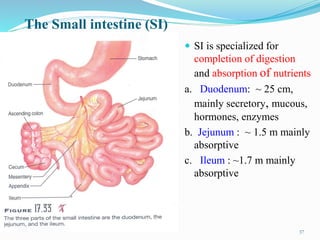
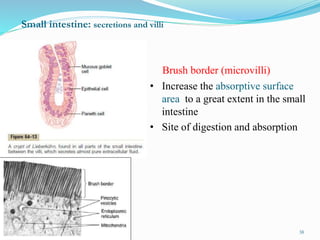
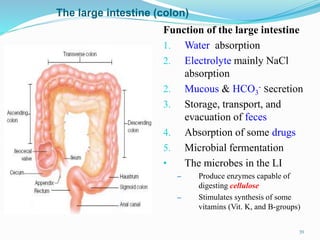
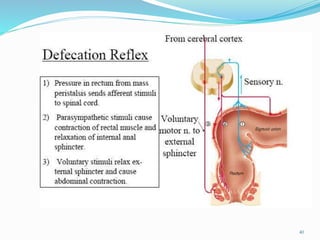
The document provides an overview of gastrointestinal physiology. It discusses the major functions of the digestive system including ingestion, digestion, absorption, and excretion. It describes the anatomy and layers of the gastrointestinal tract from the mouth to anus. Key sections include descriptions of motility in different parts of the GI tract, the secretions of saliva, gastric juices, bile, pancreatic juices and intestinal secretions. It also briefly discusses common GI disorders.