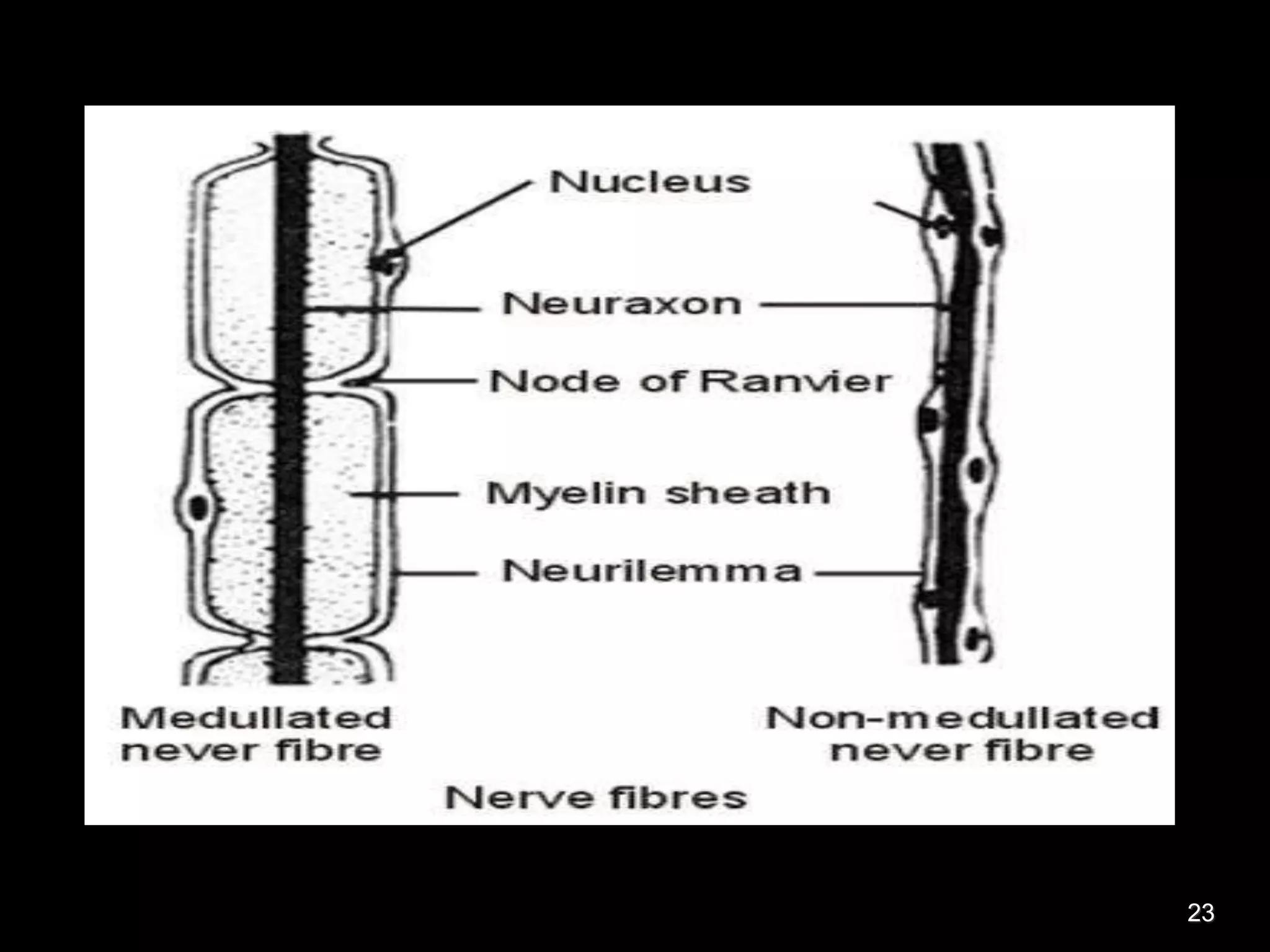
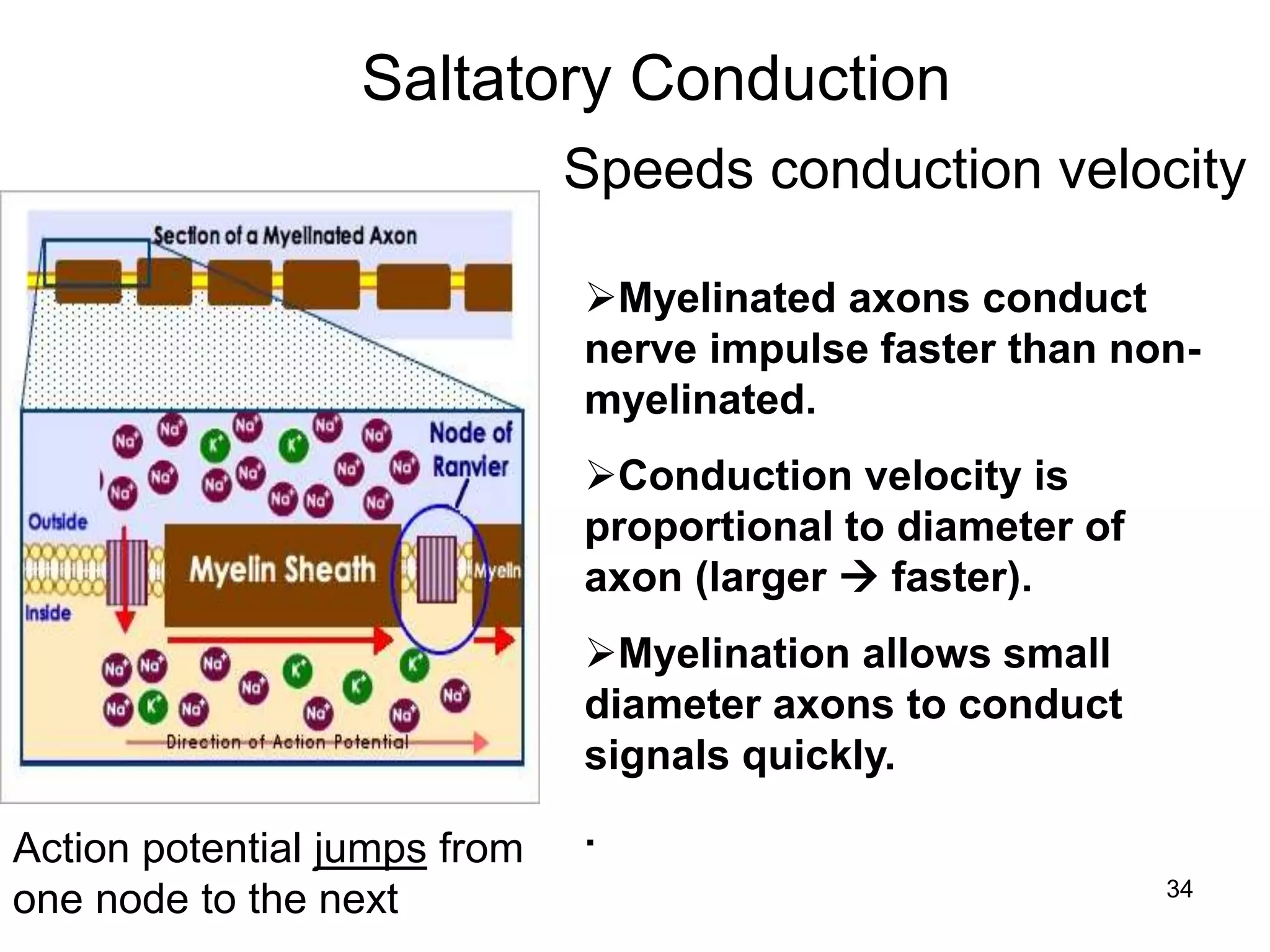
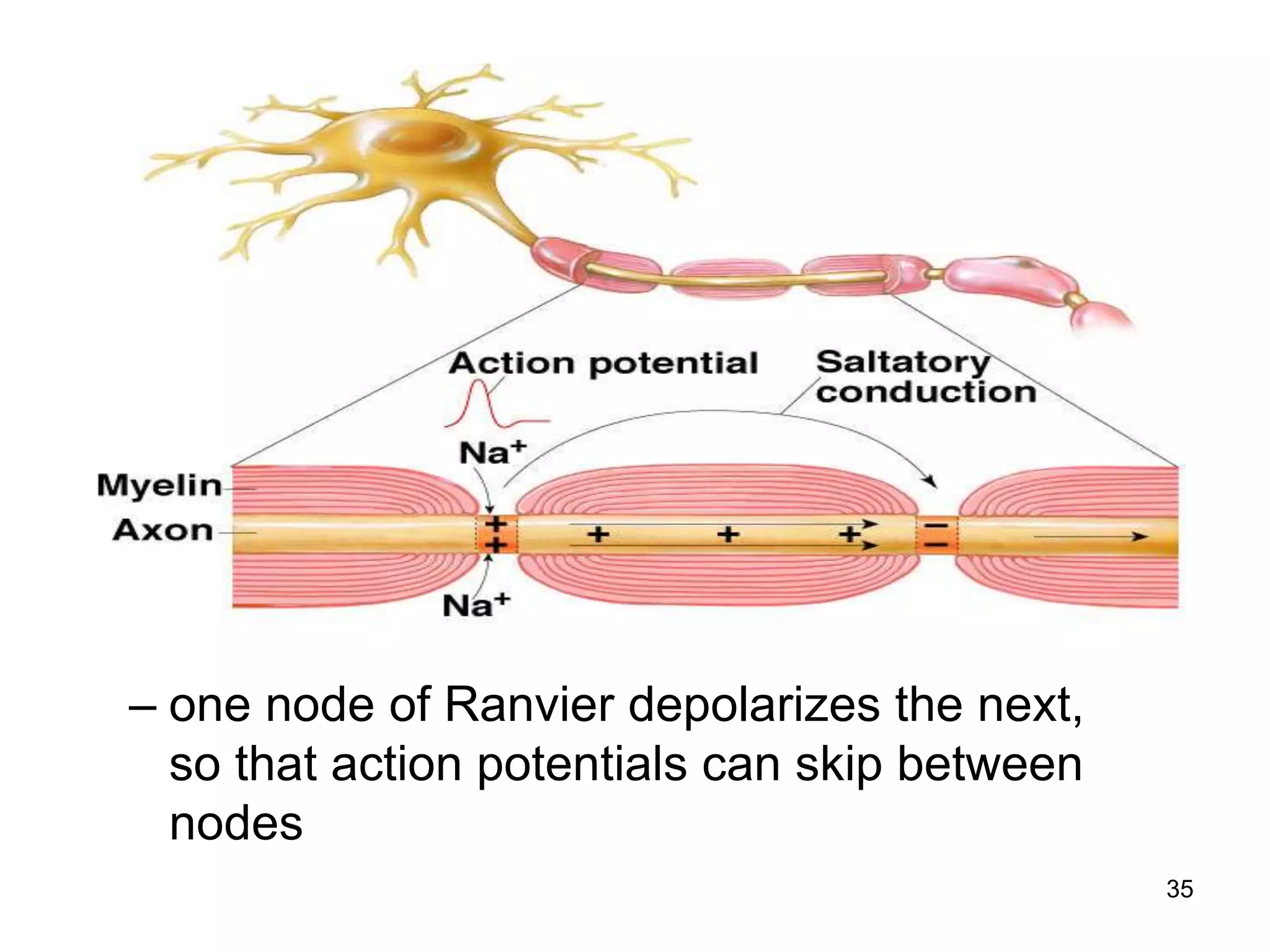
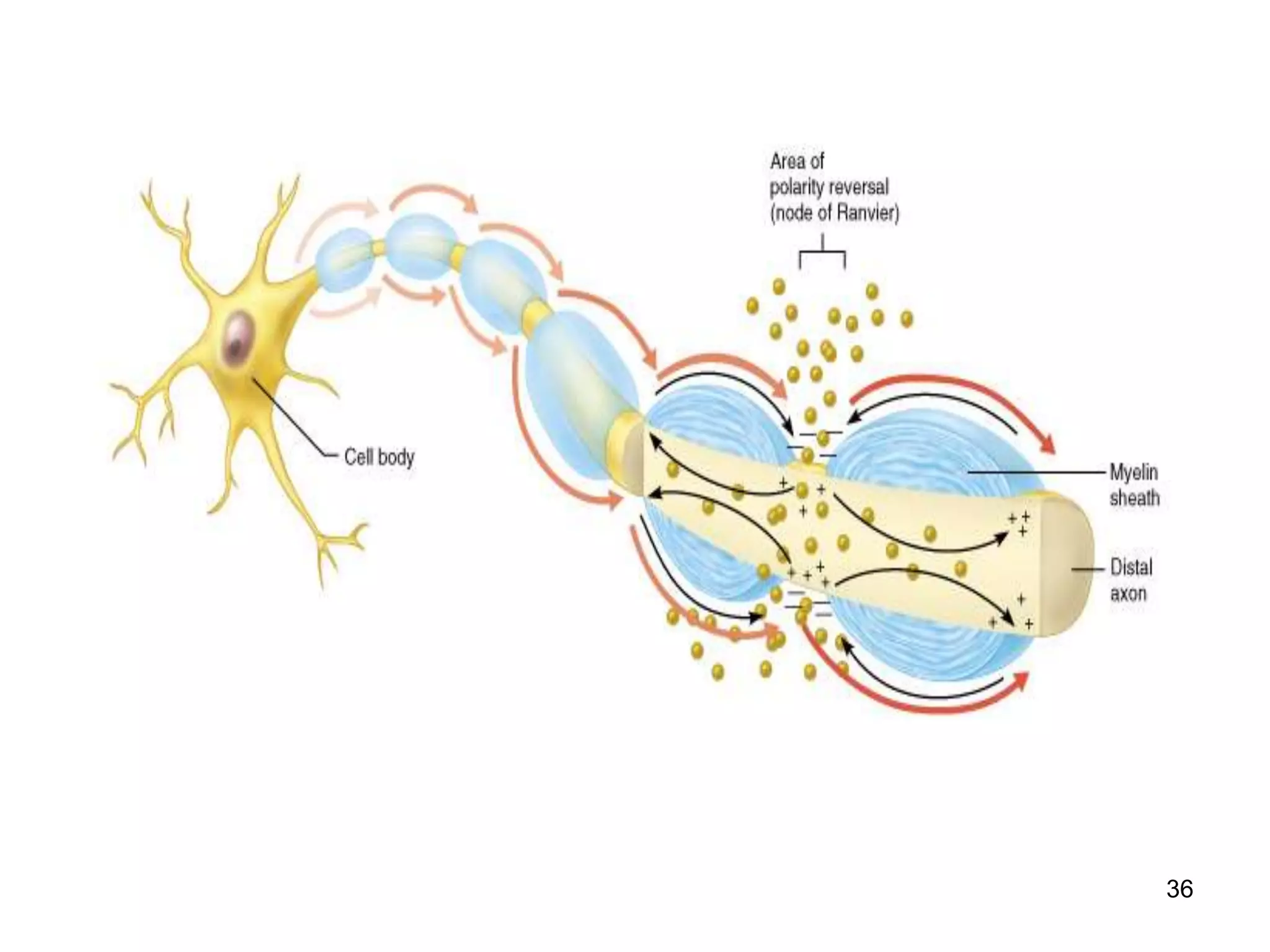
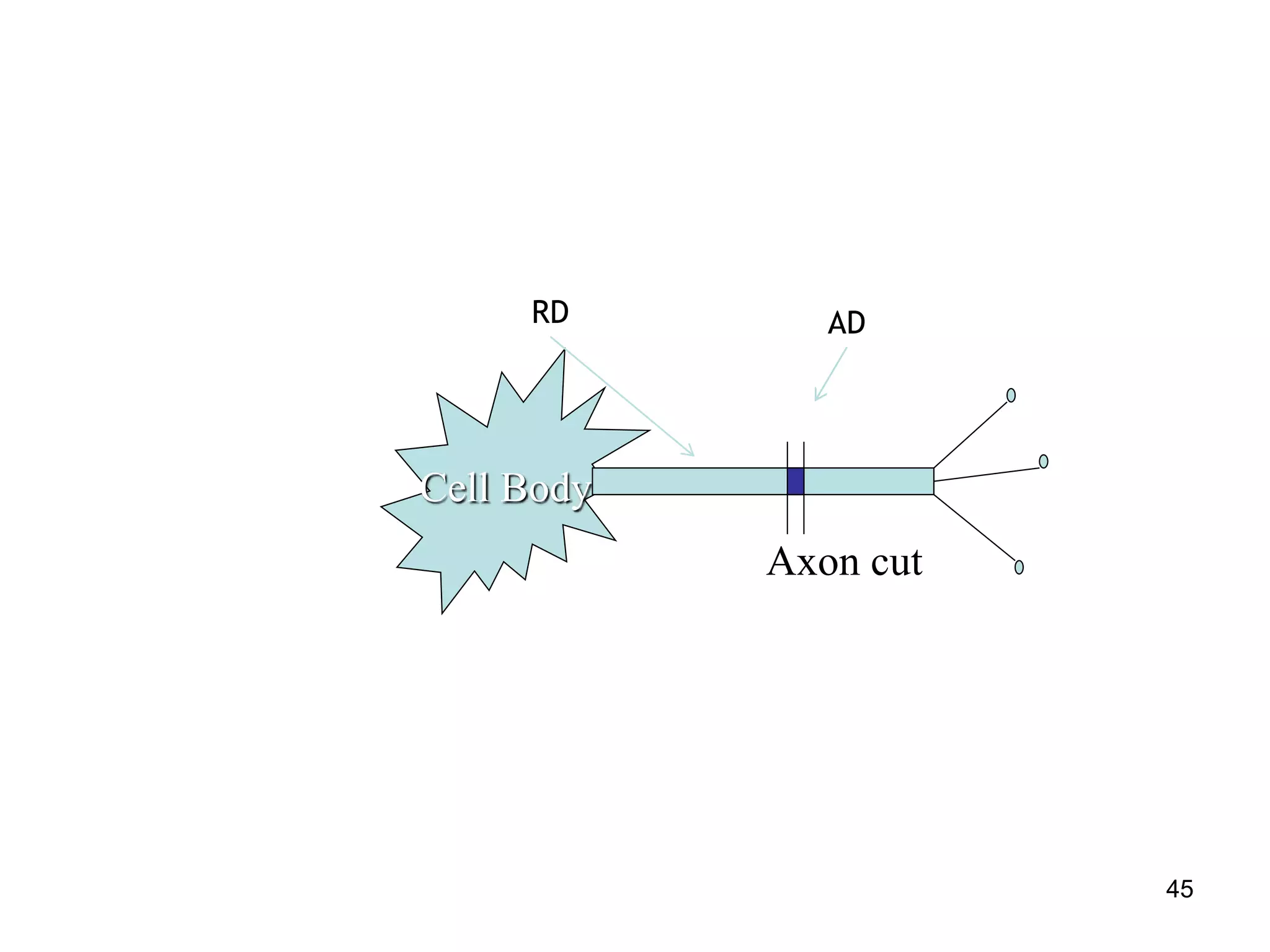
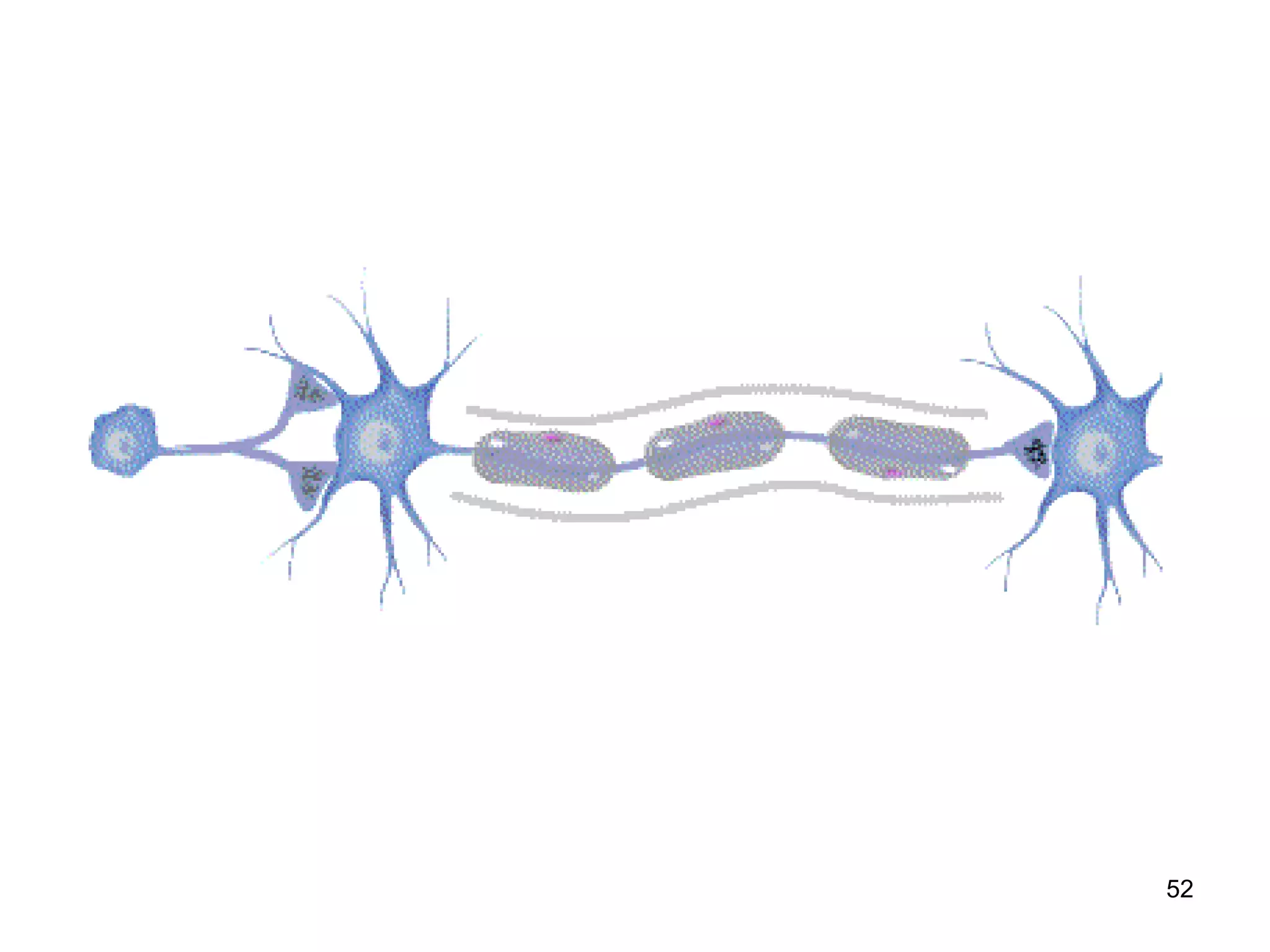
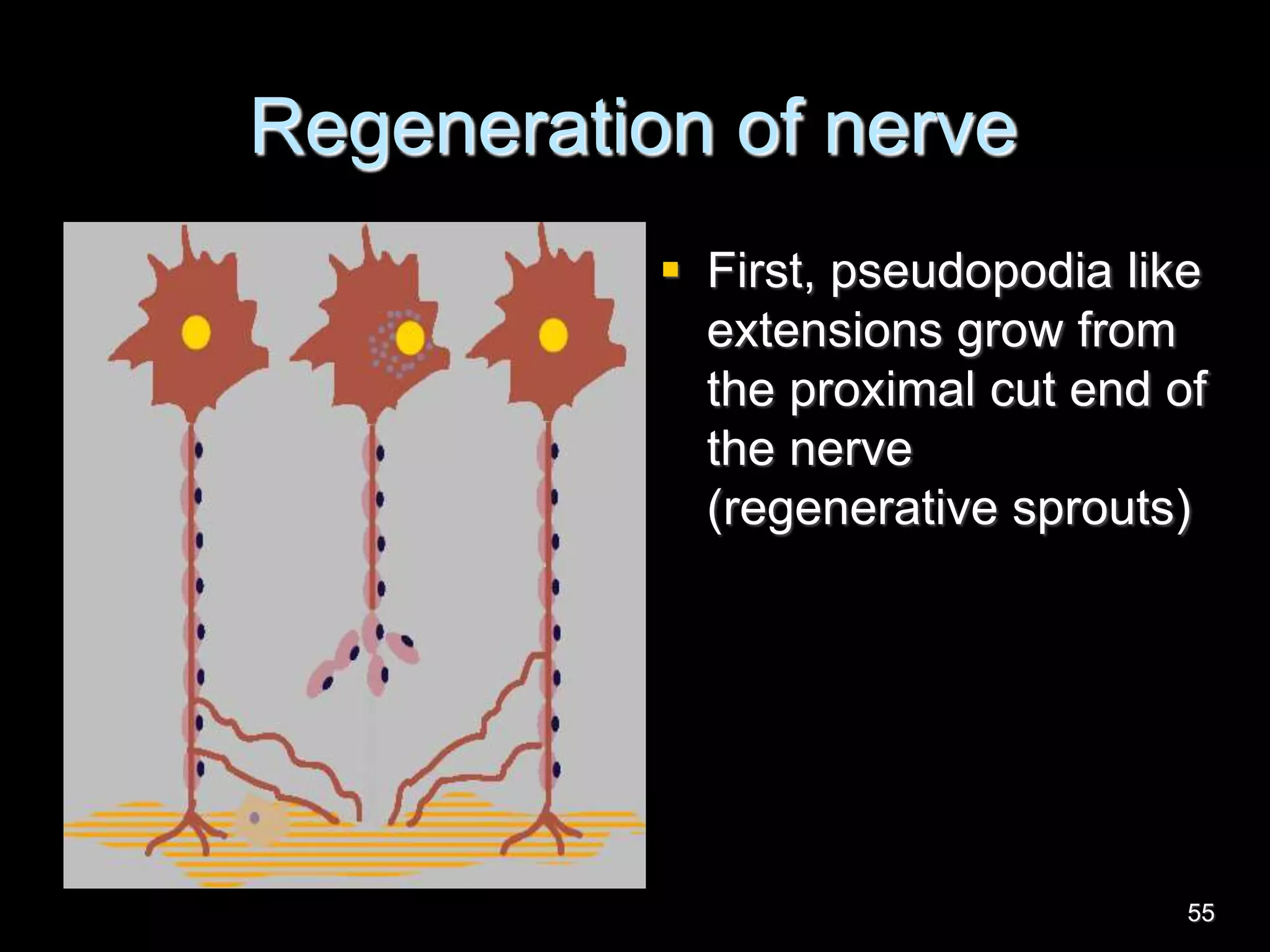
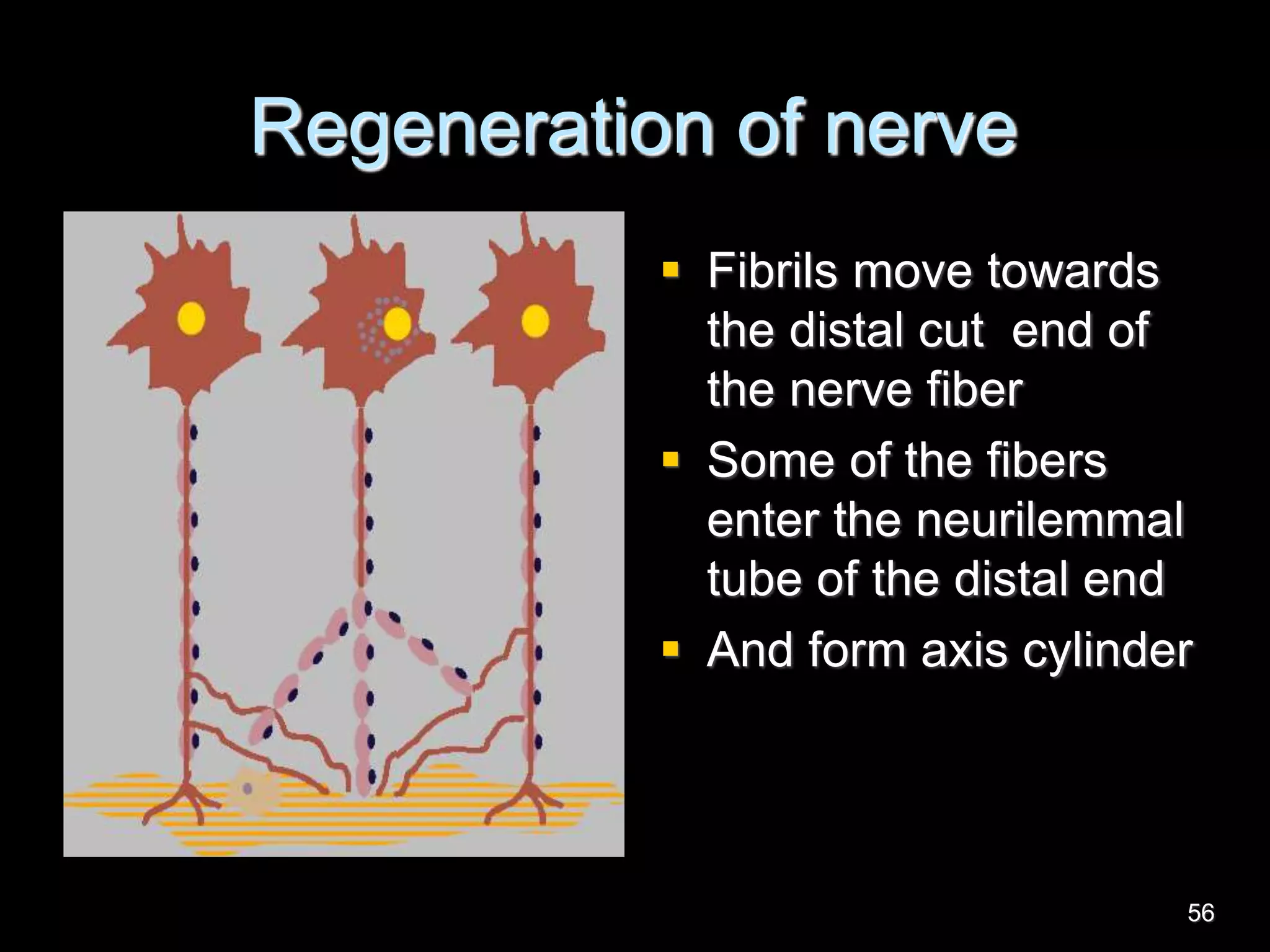
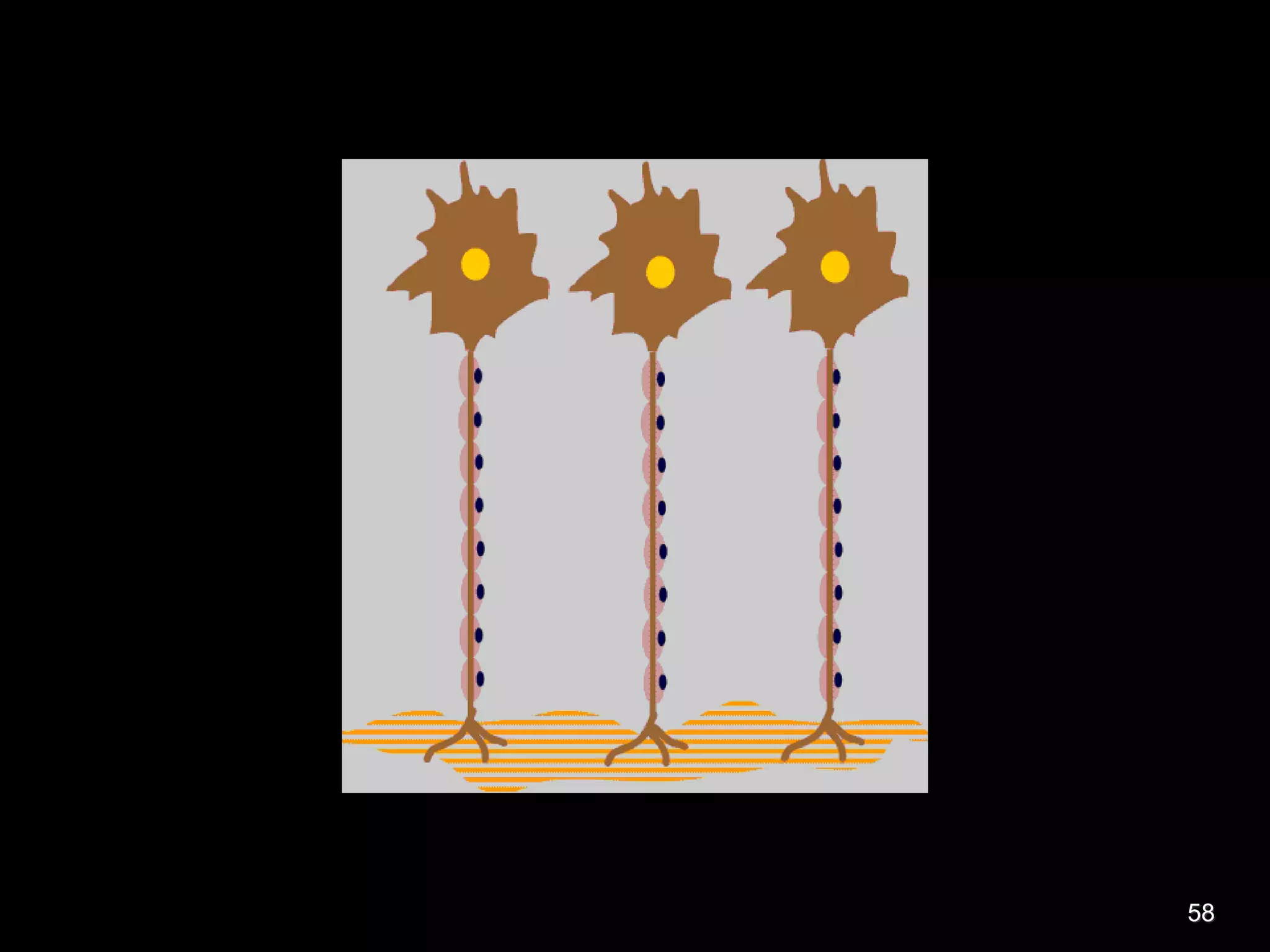
Nerve fibers are classified based on their structure, distribution, origin and function. They can be myelinated or unmyelinated. When injured, the distal portion undergoes Wallerian degeneration over 3 months as the axon and myelin sheath break down. The cell body shows chromatolysis. Regeneration is possible if the nerve ends are close together. New axonal growth occurs rapidly, entering the distal stump at 3-4mm/day. Myelination resumes over a year. Though anatomy recovers, full function returns slowly.