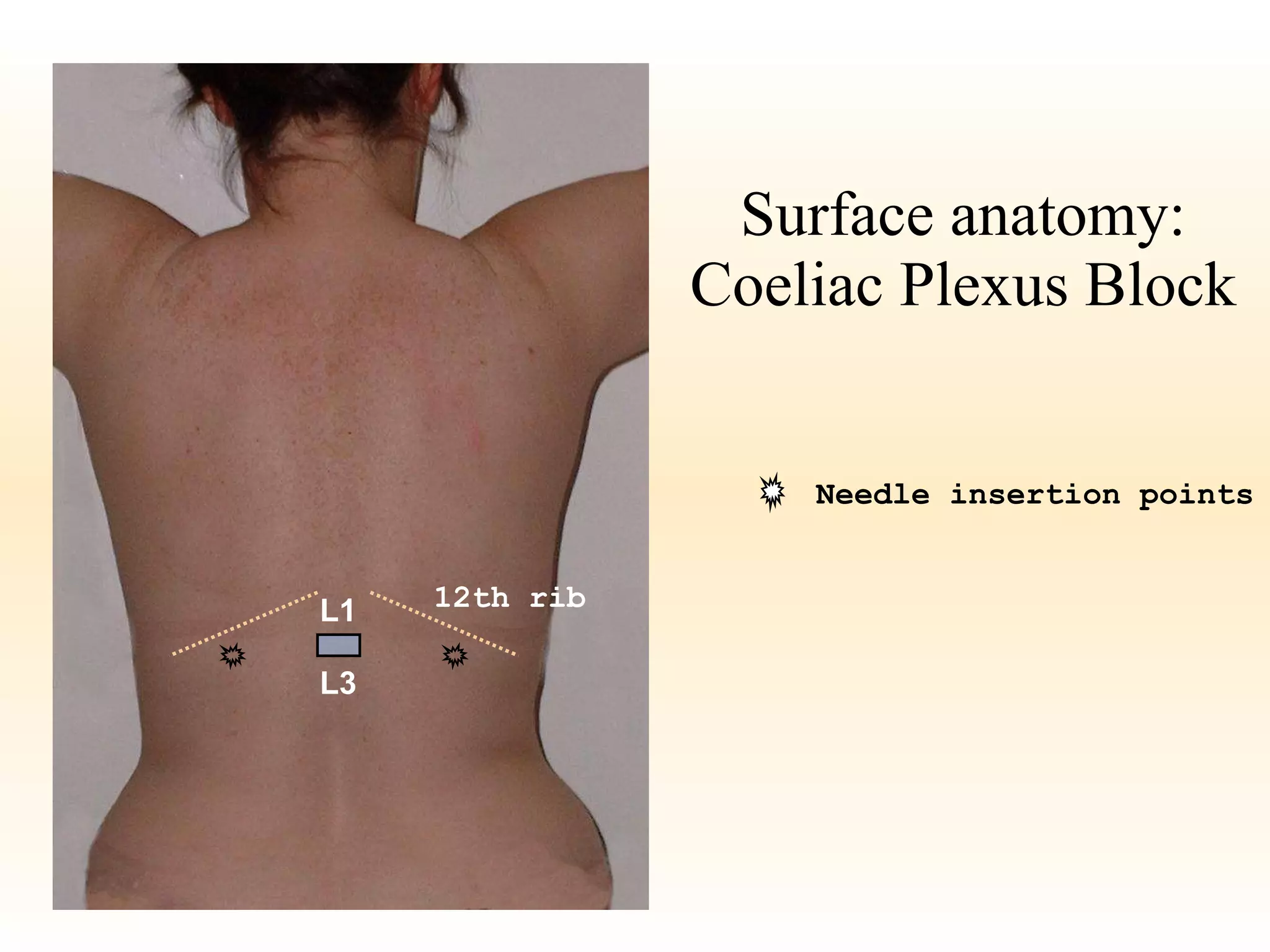
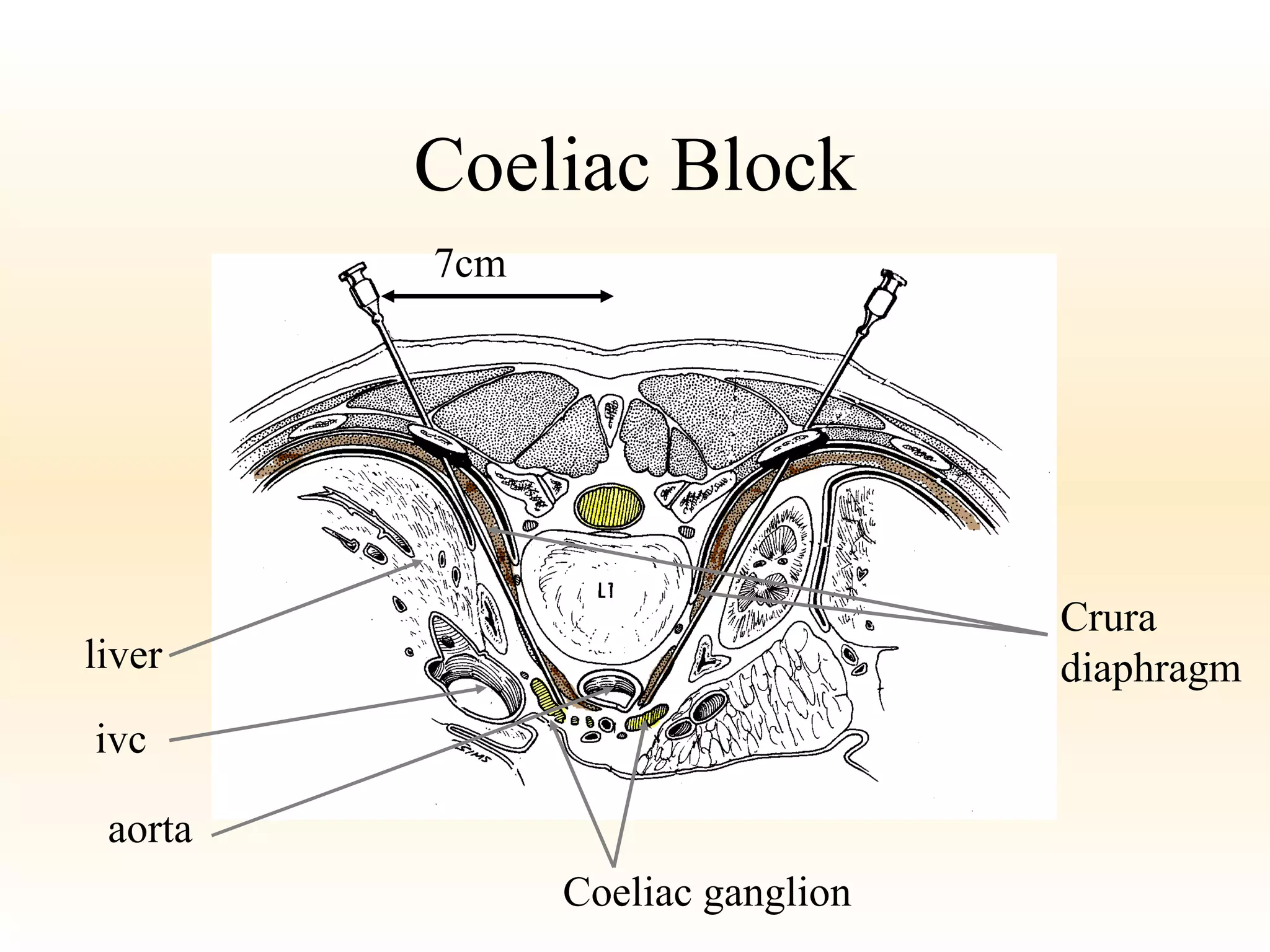
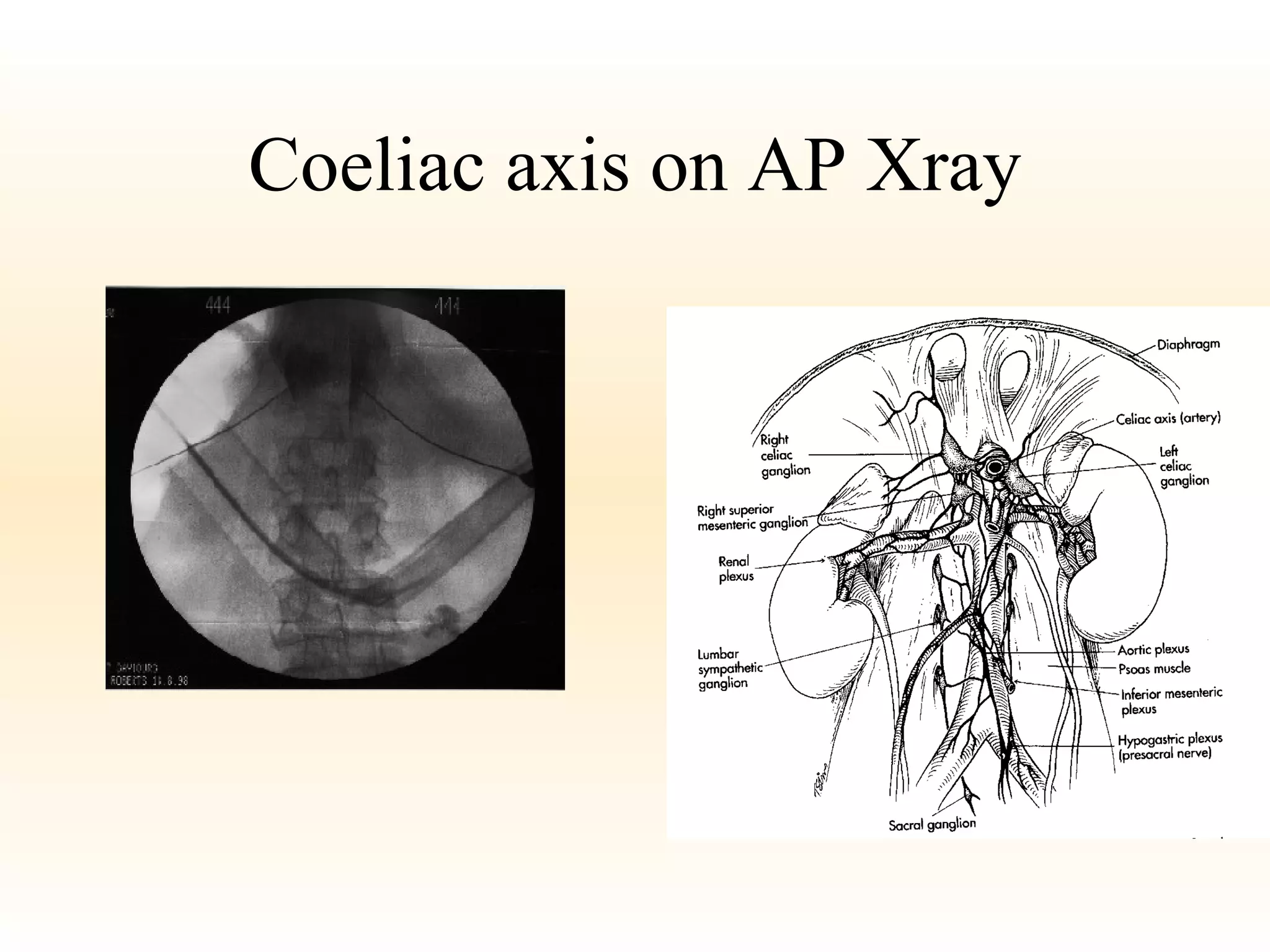
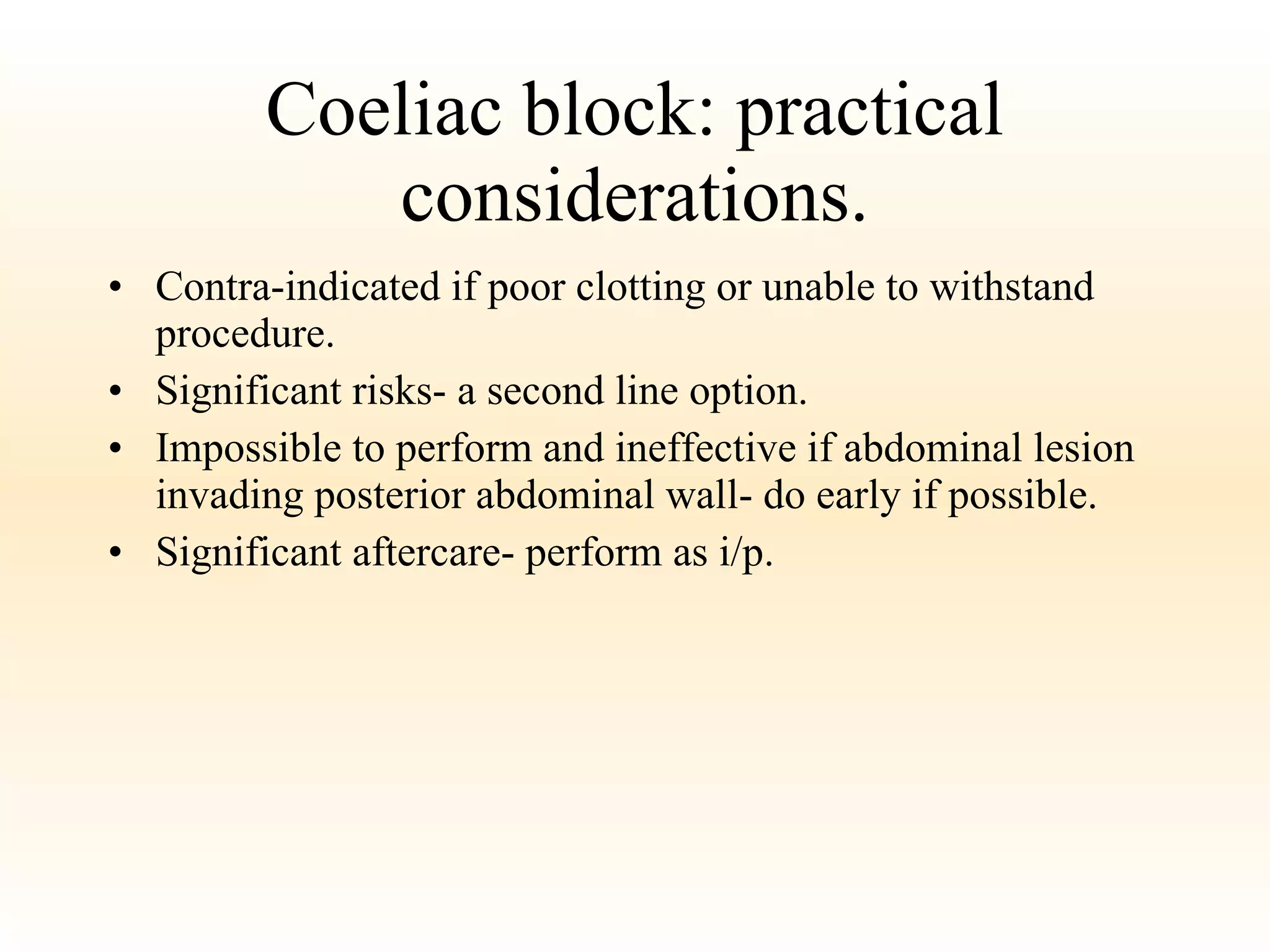
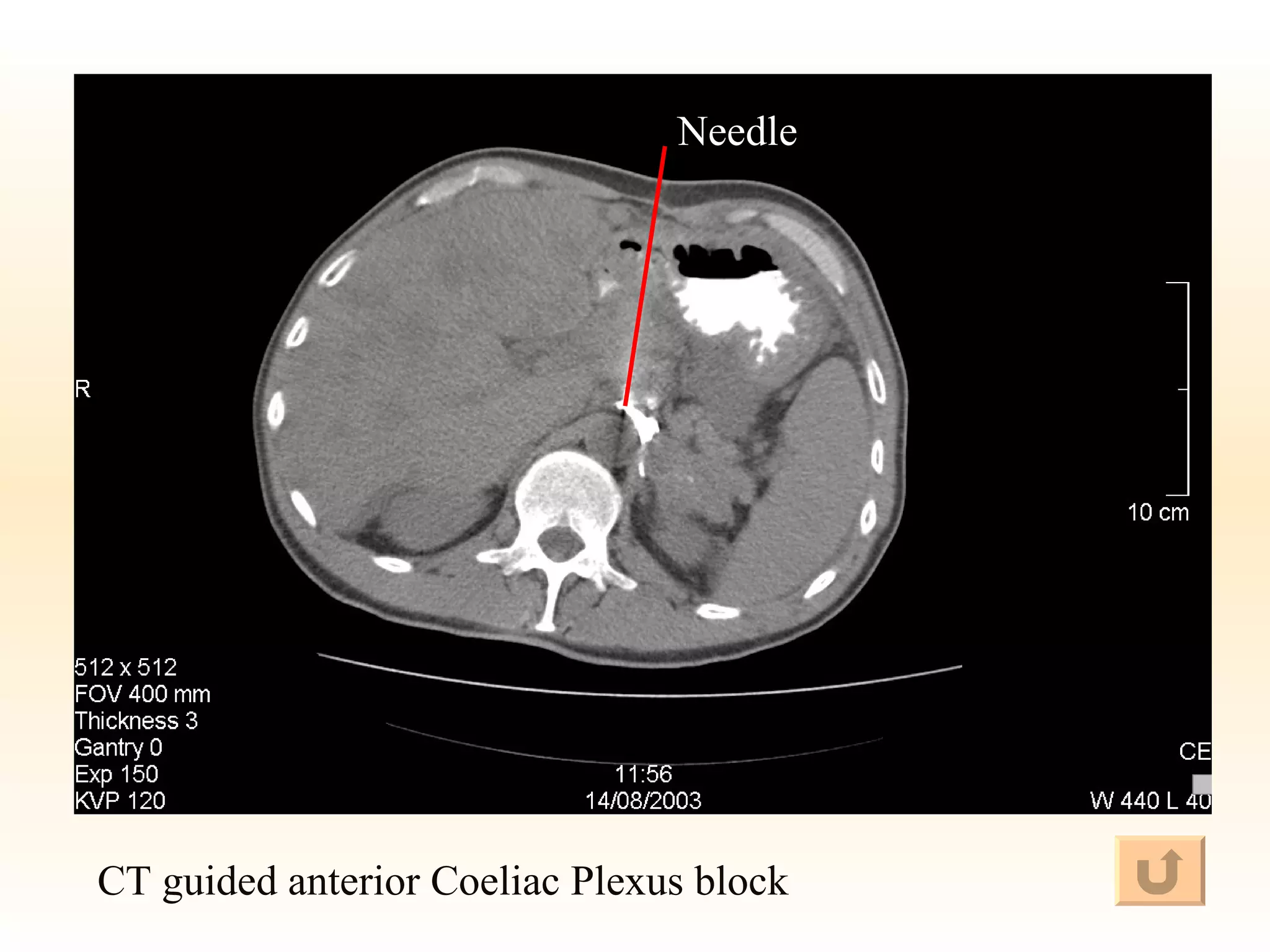
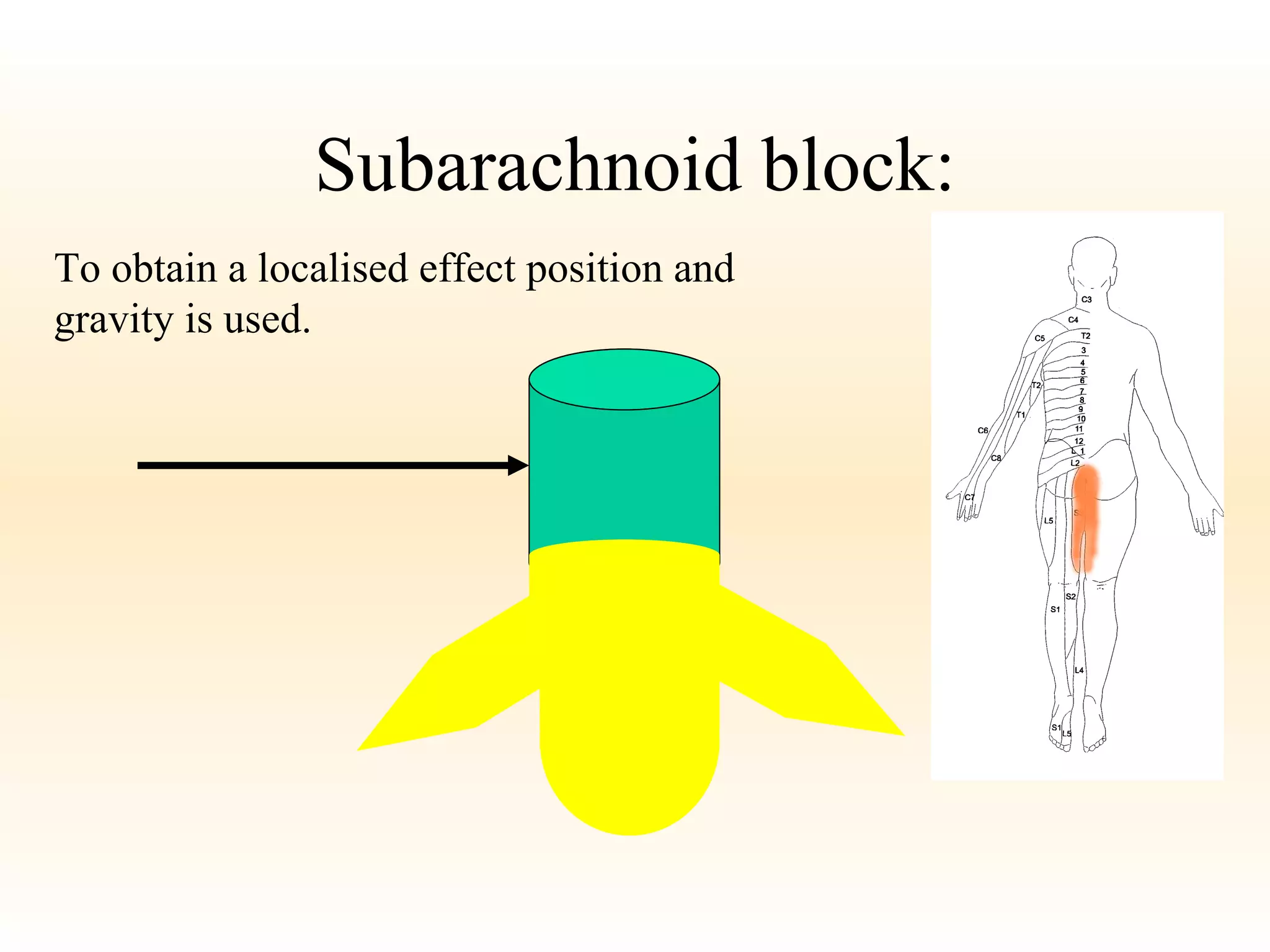
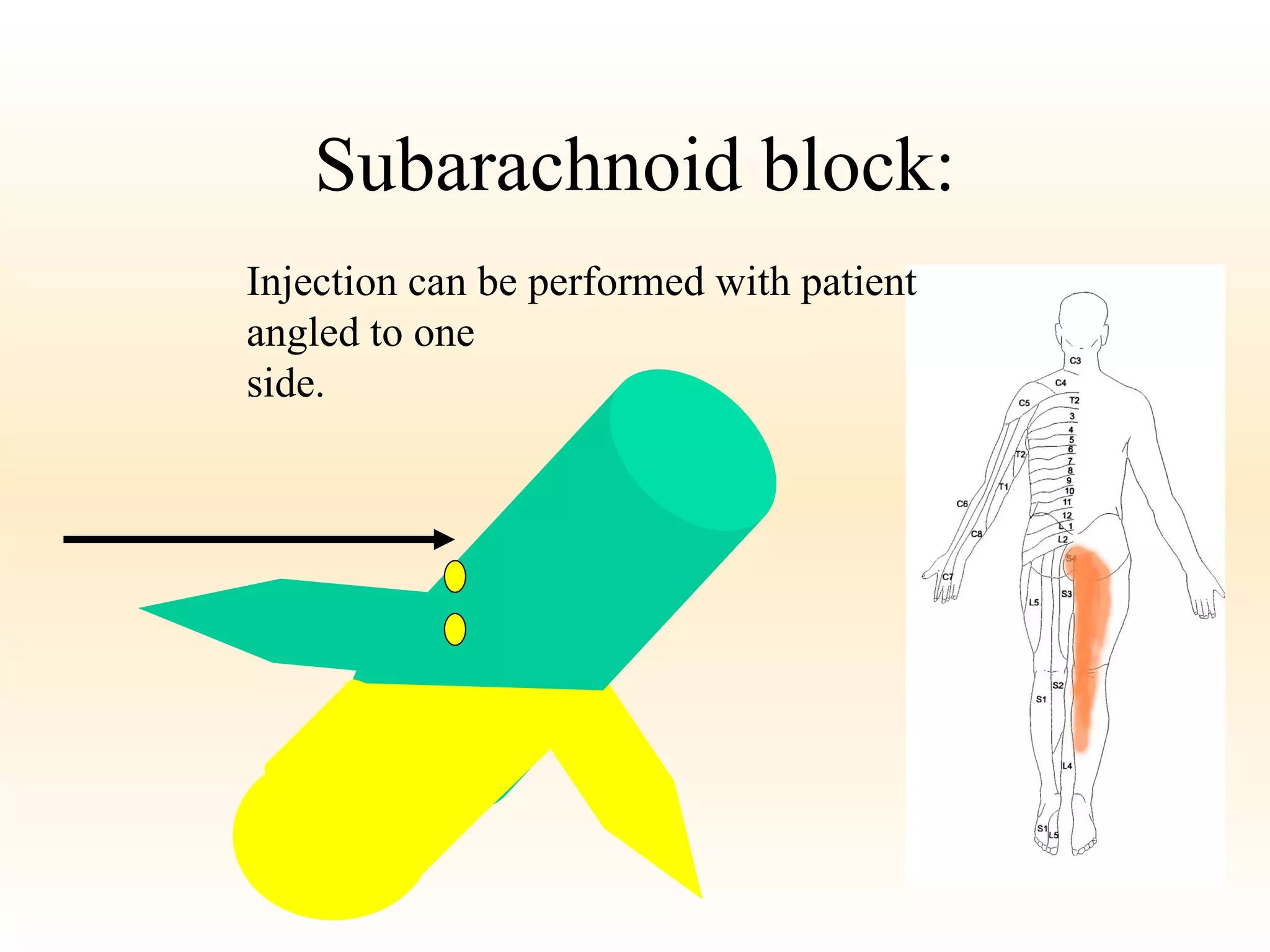
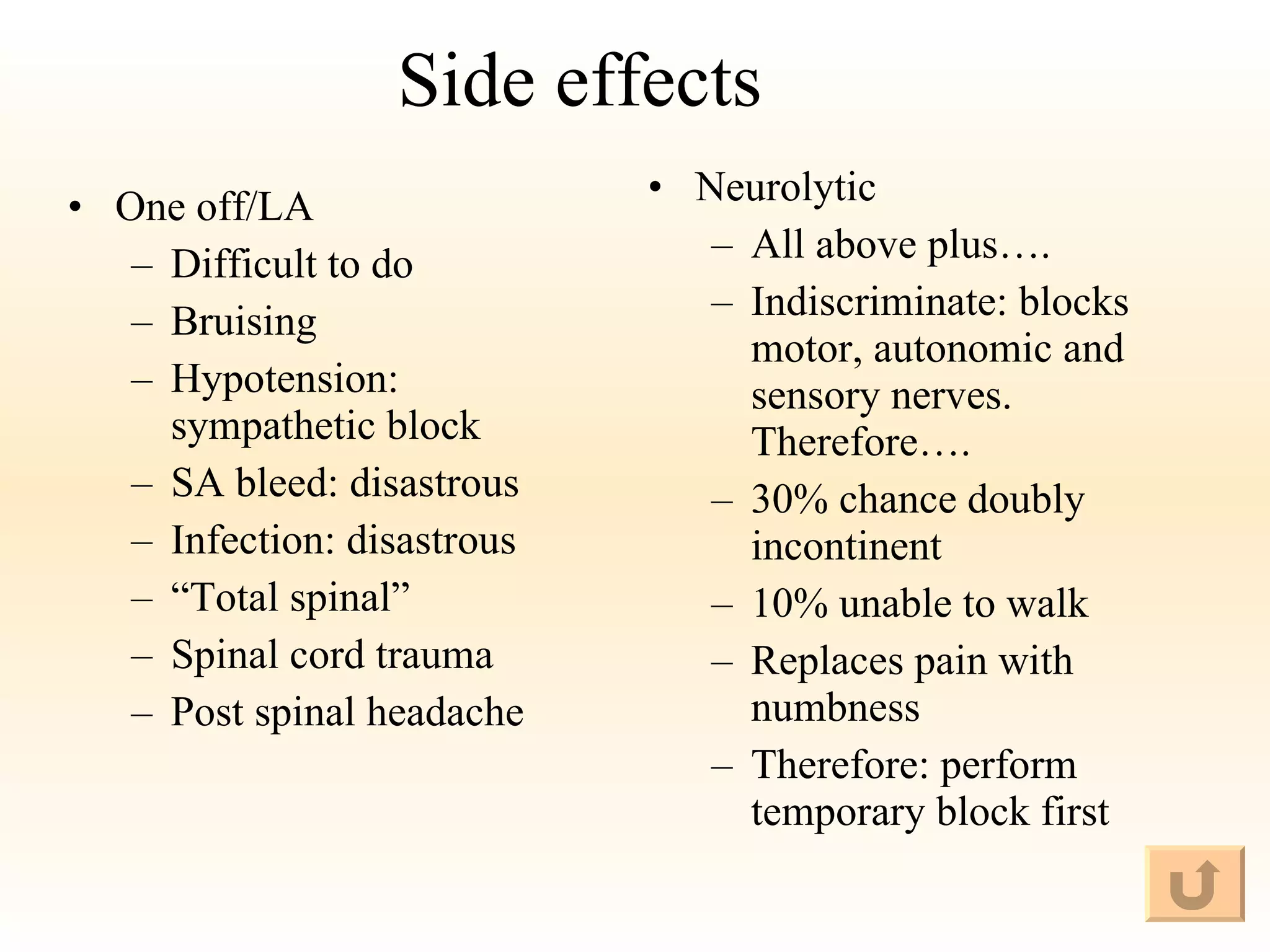
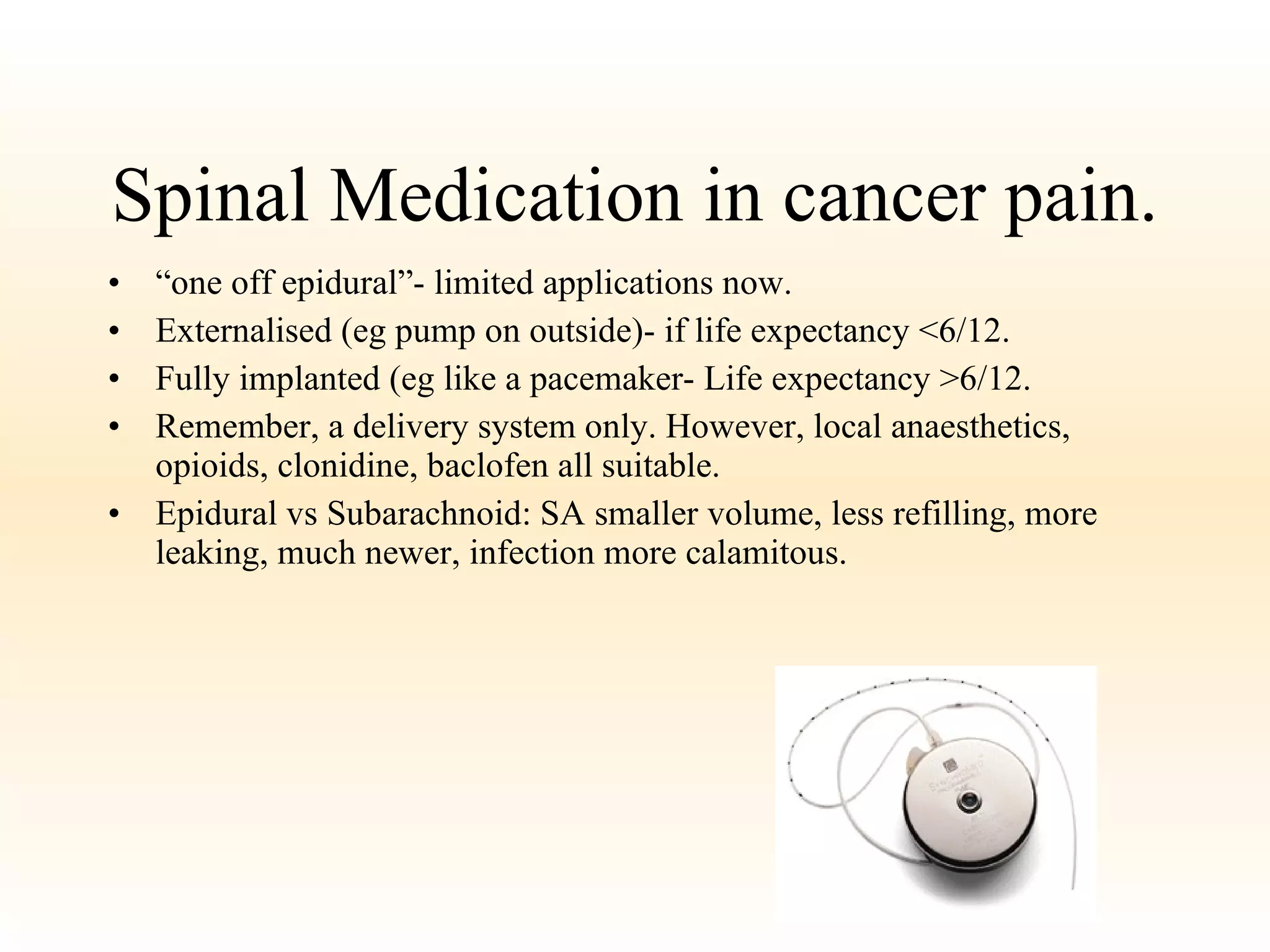
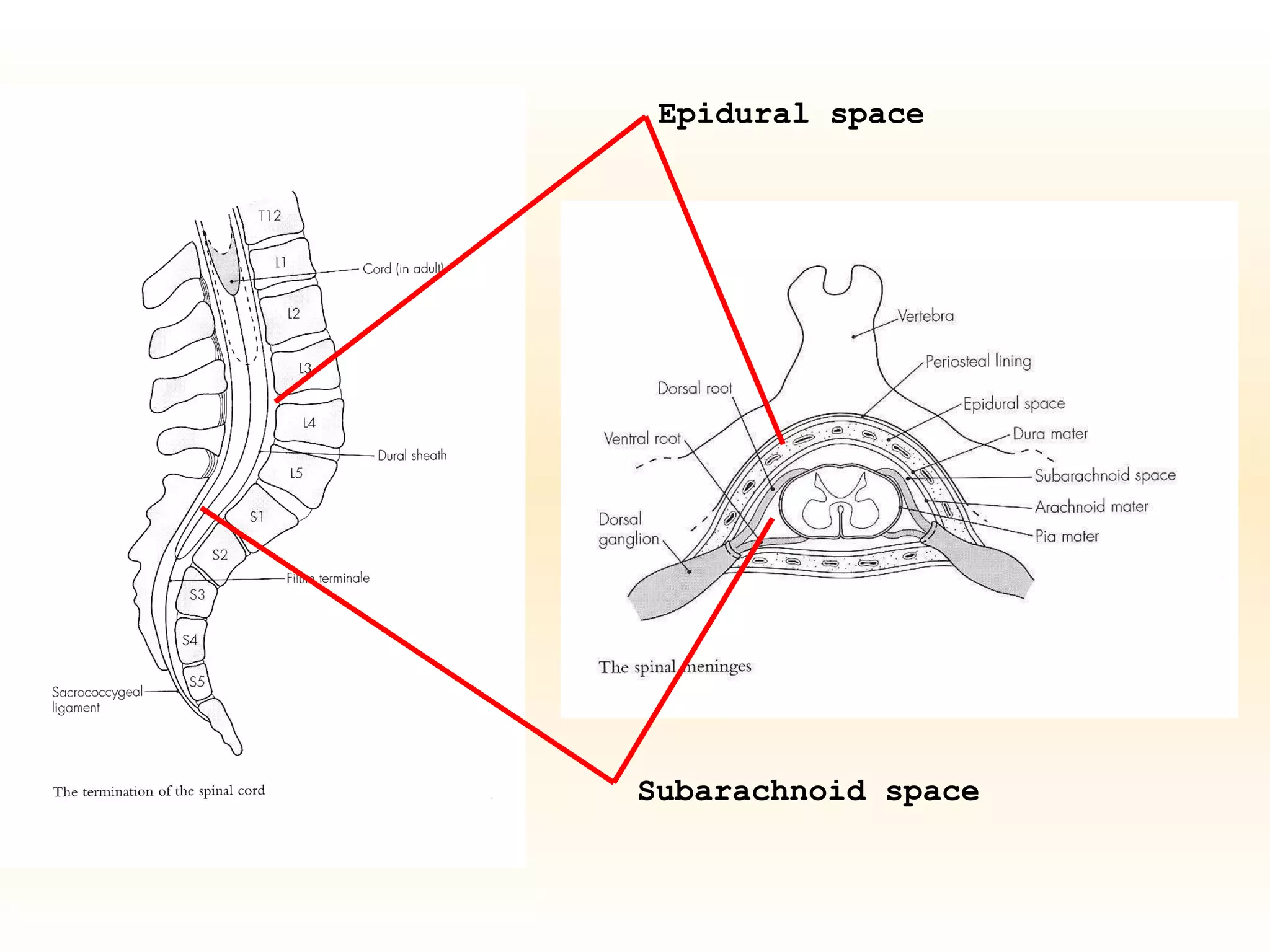
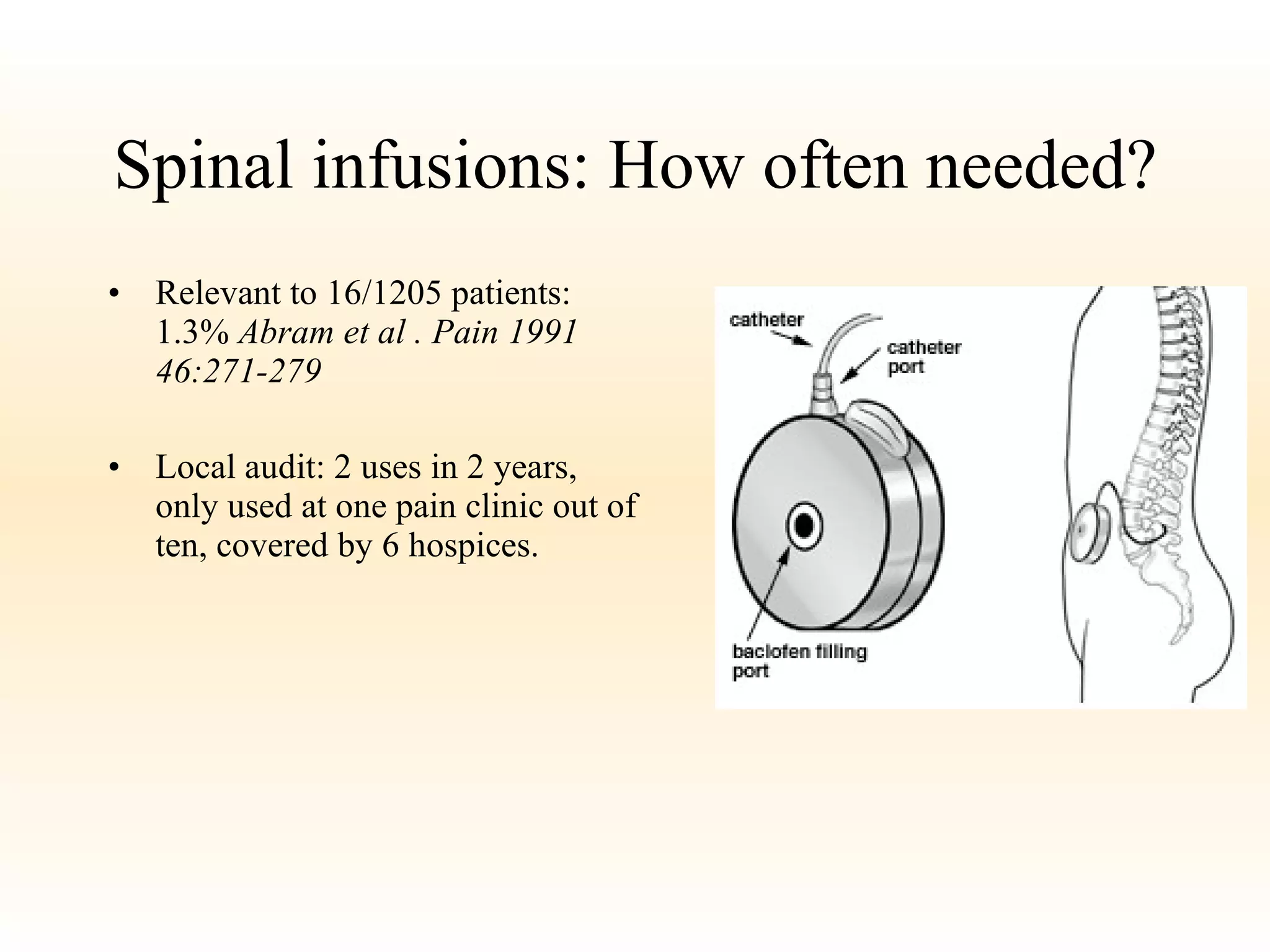
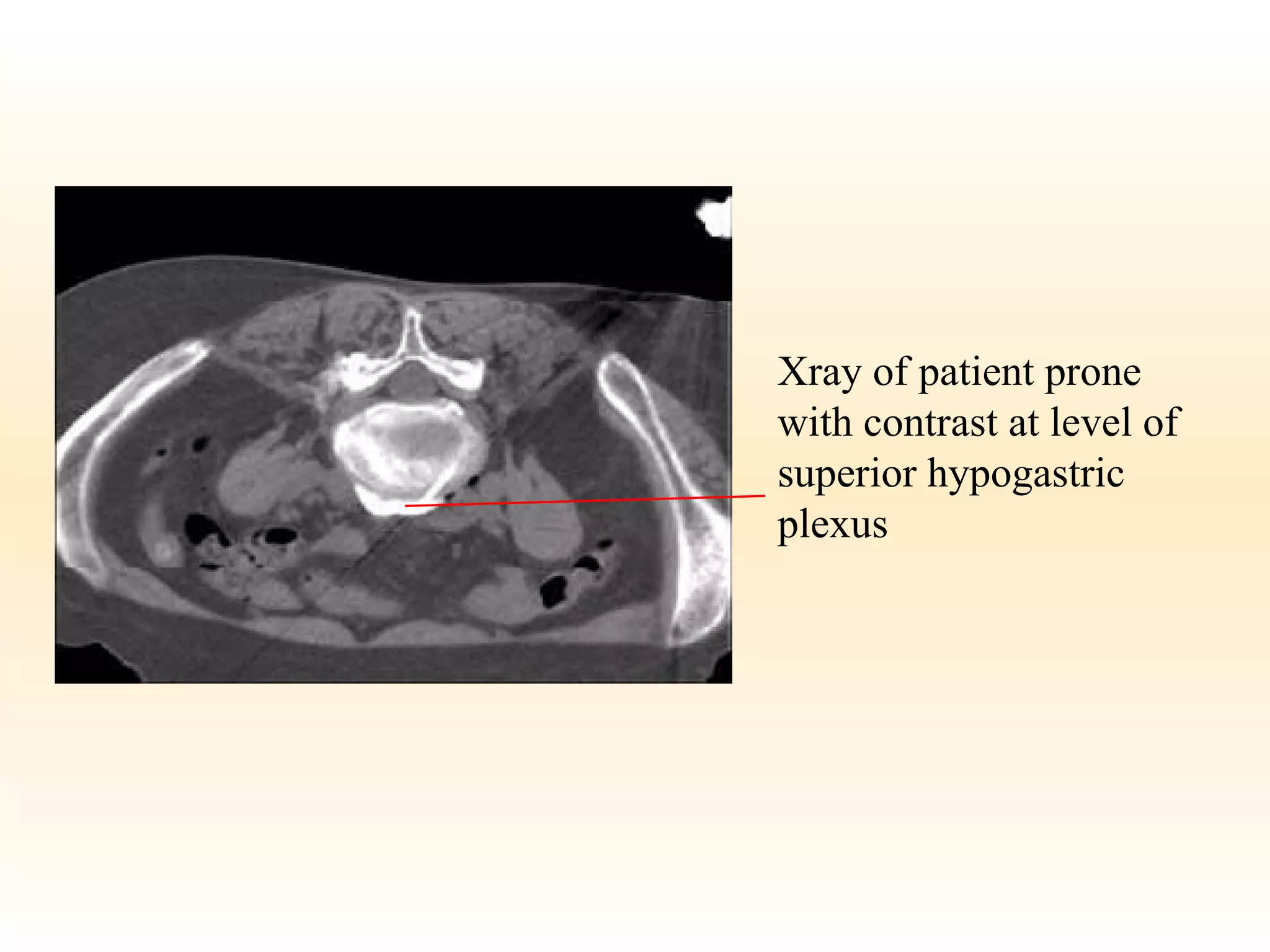
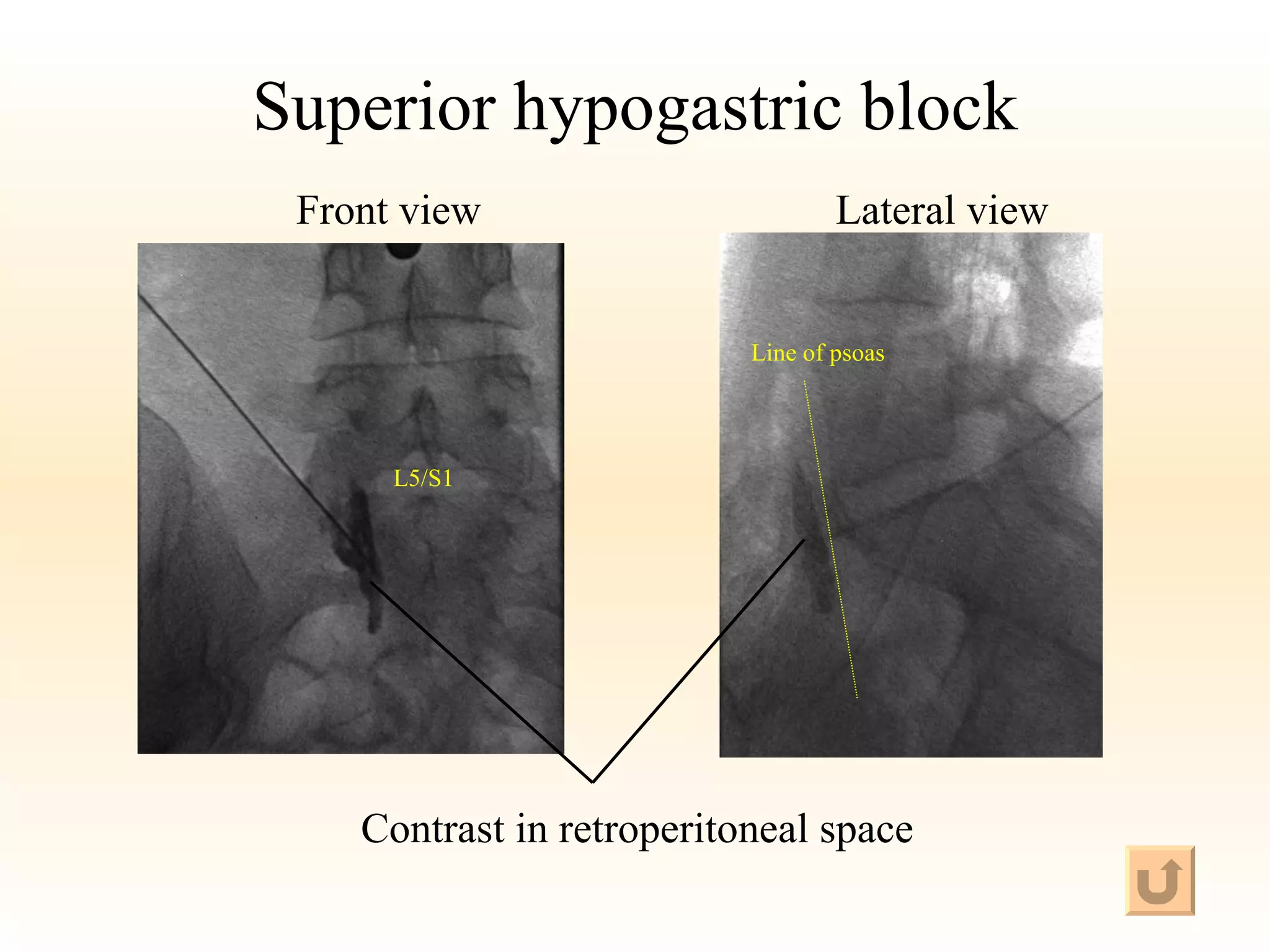
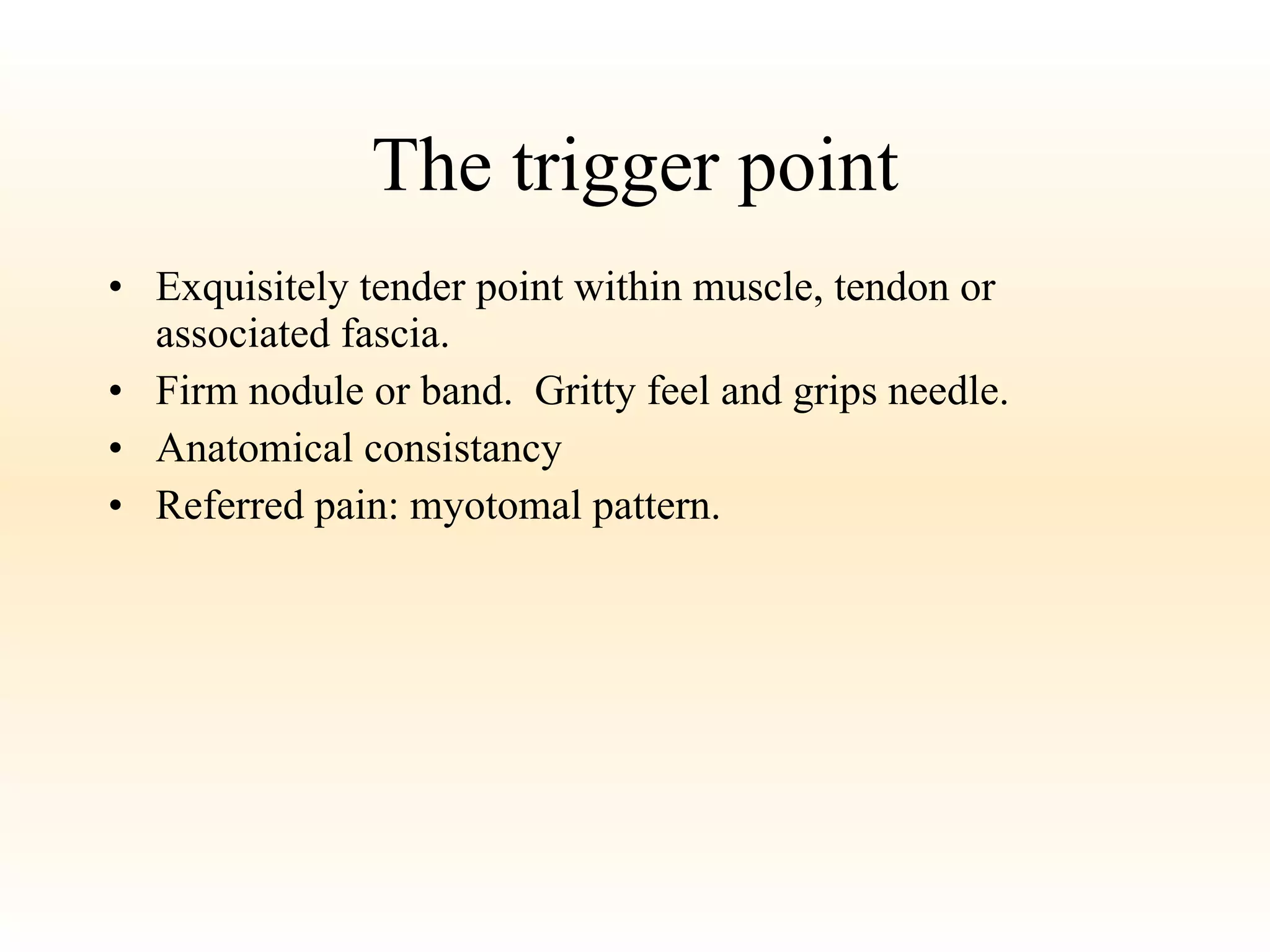
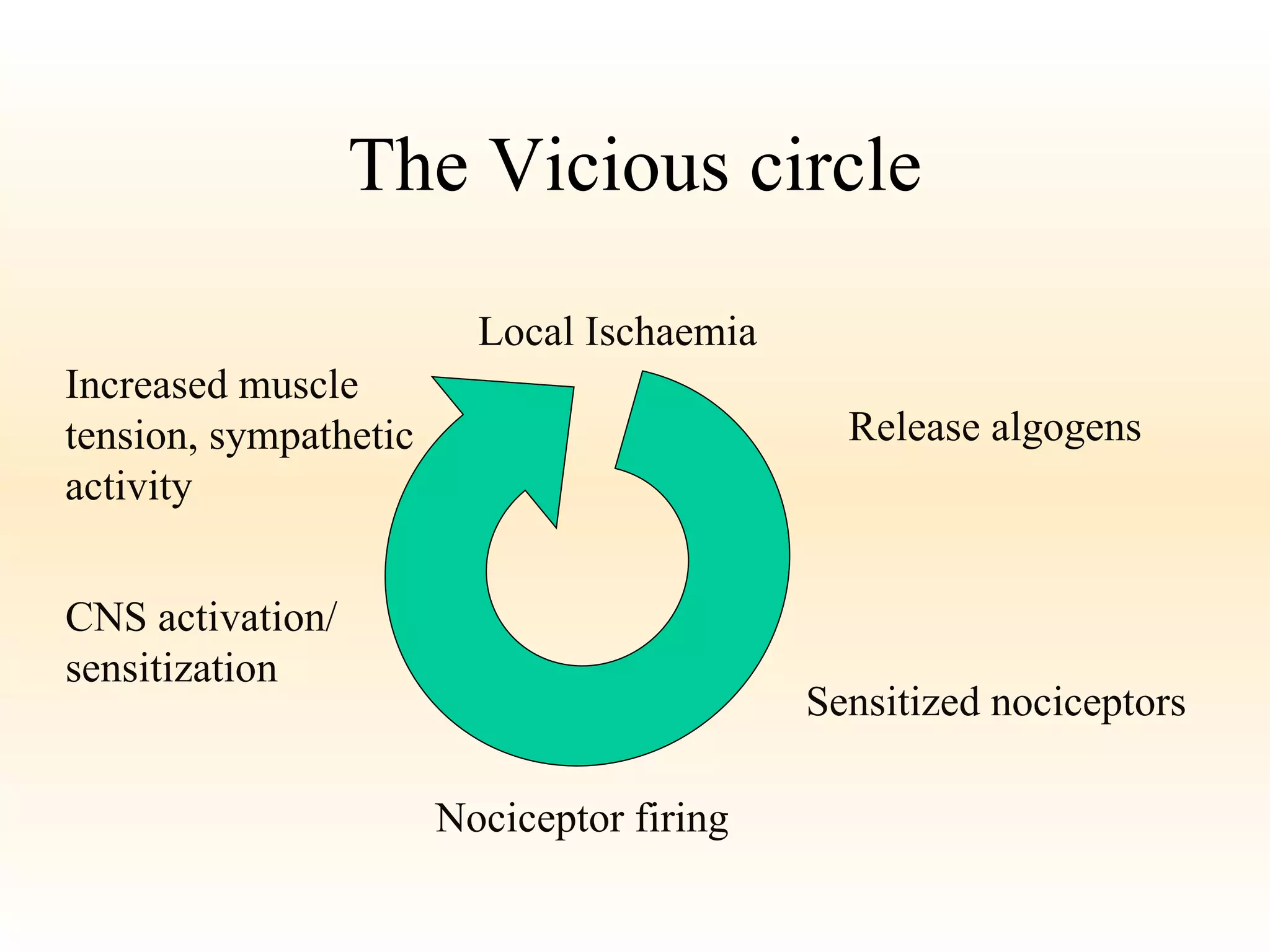
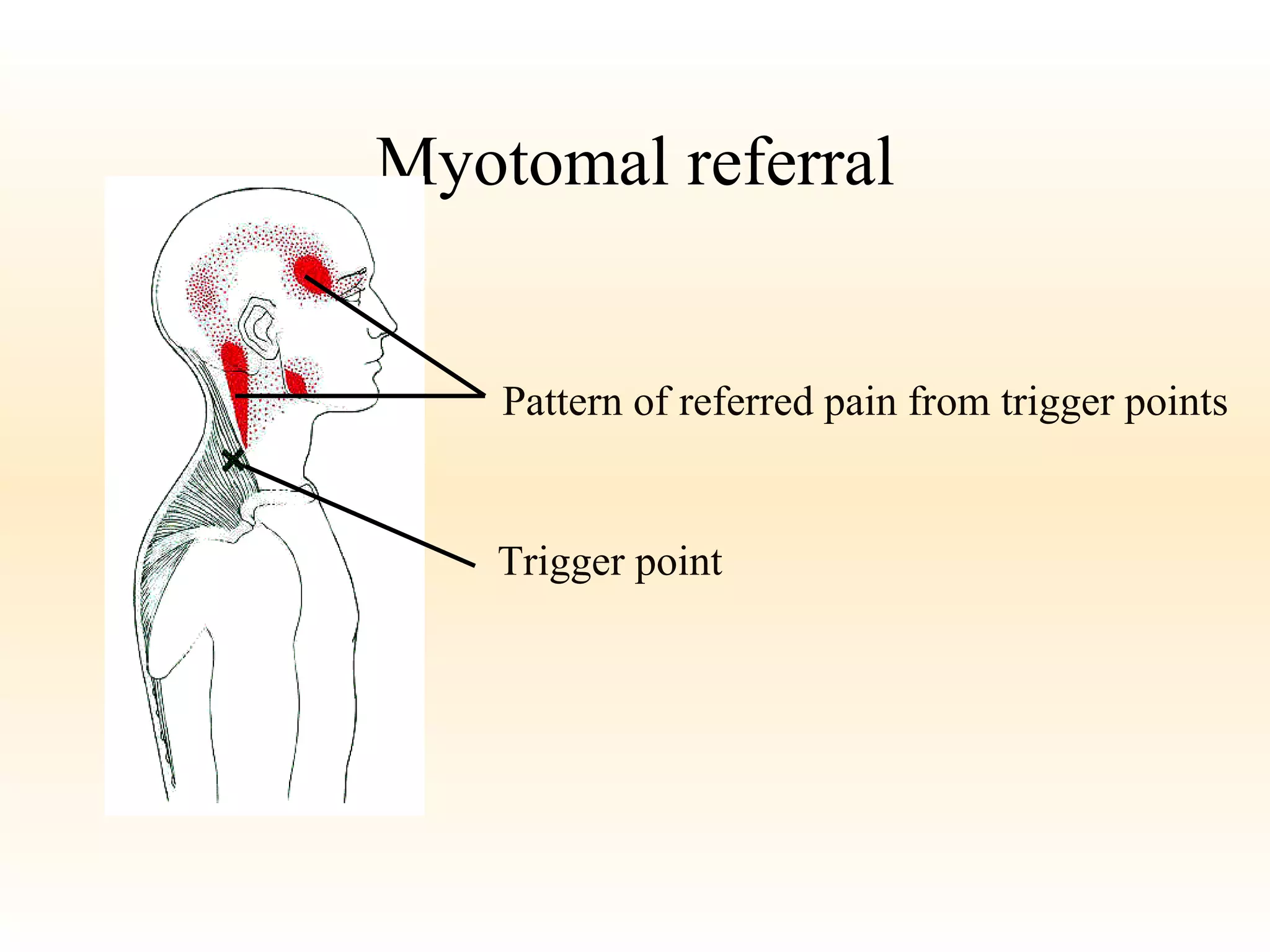
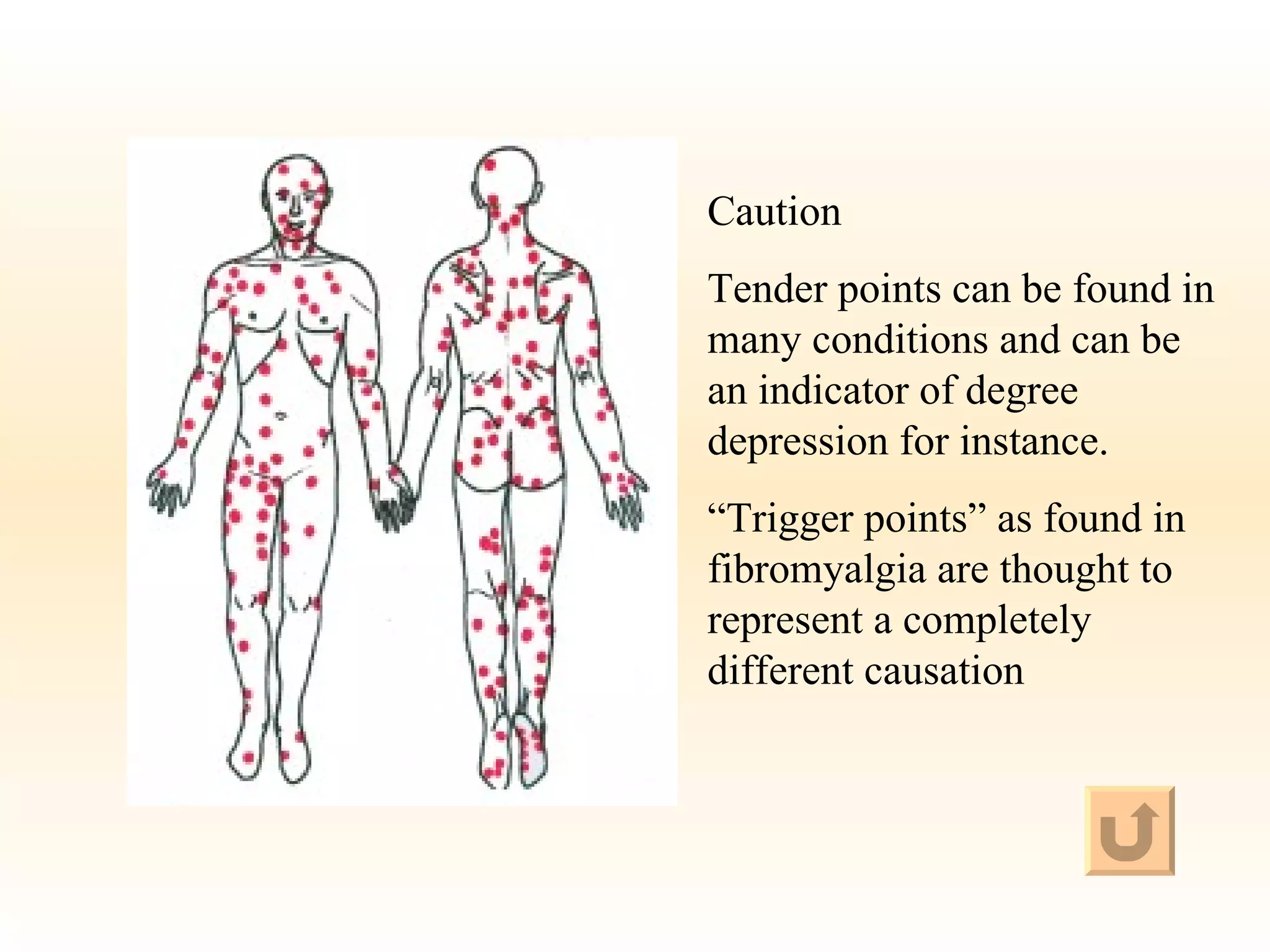
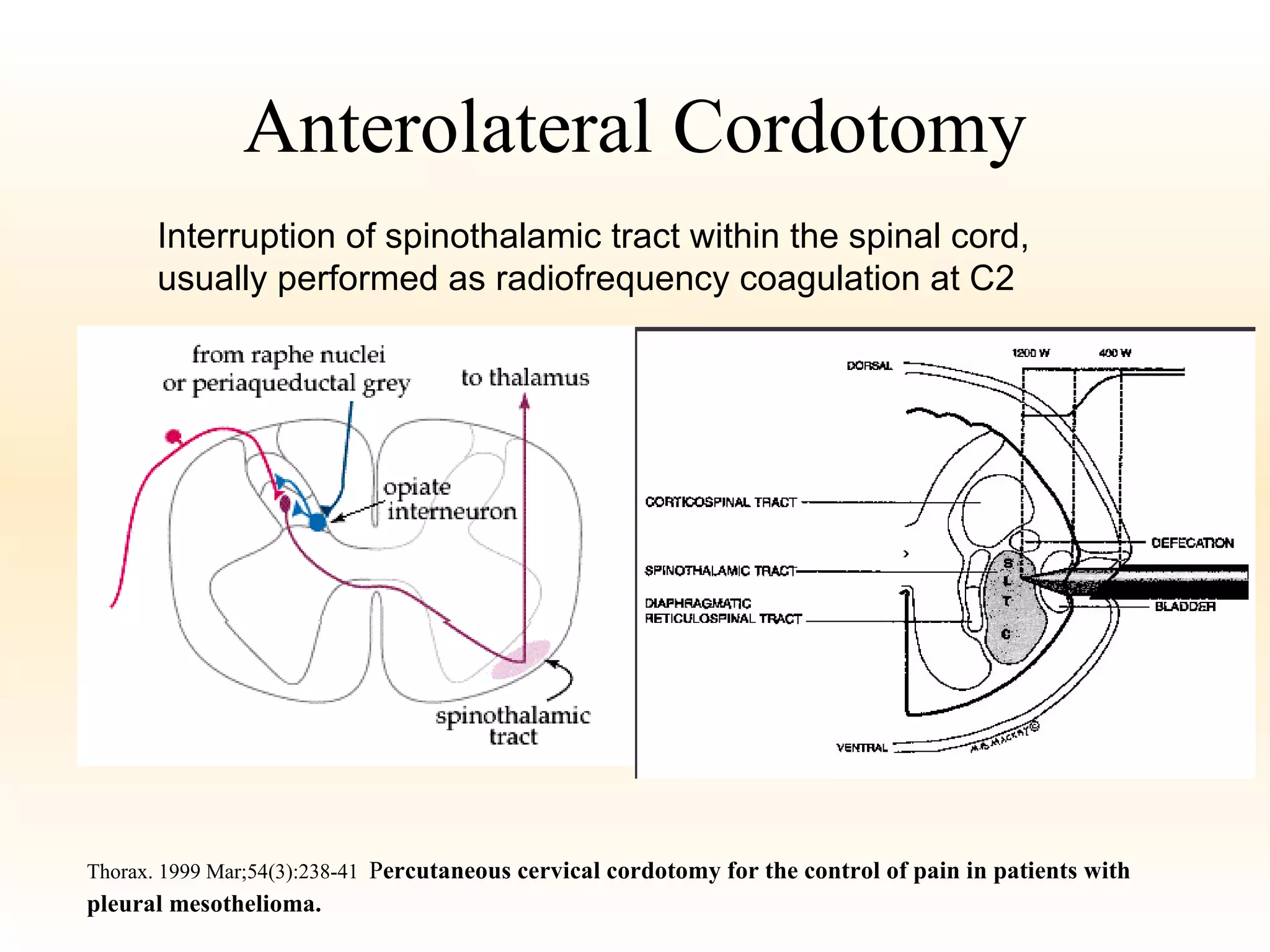
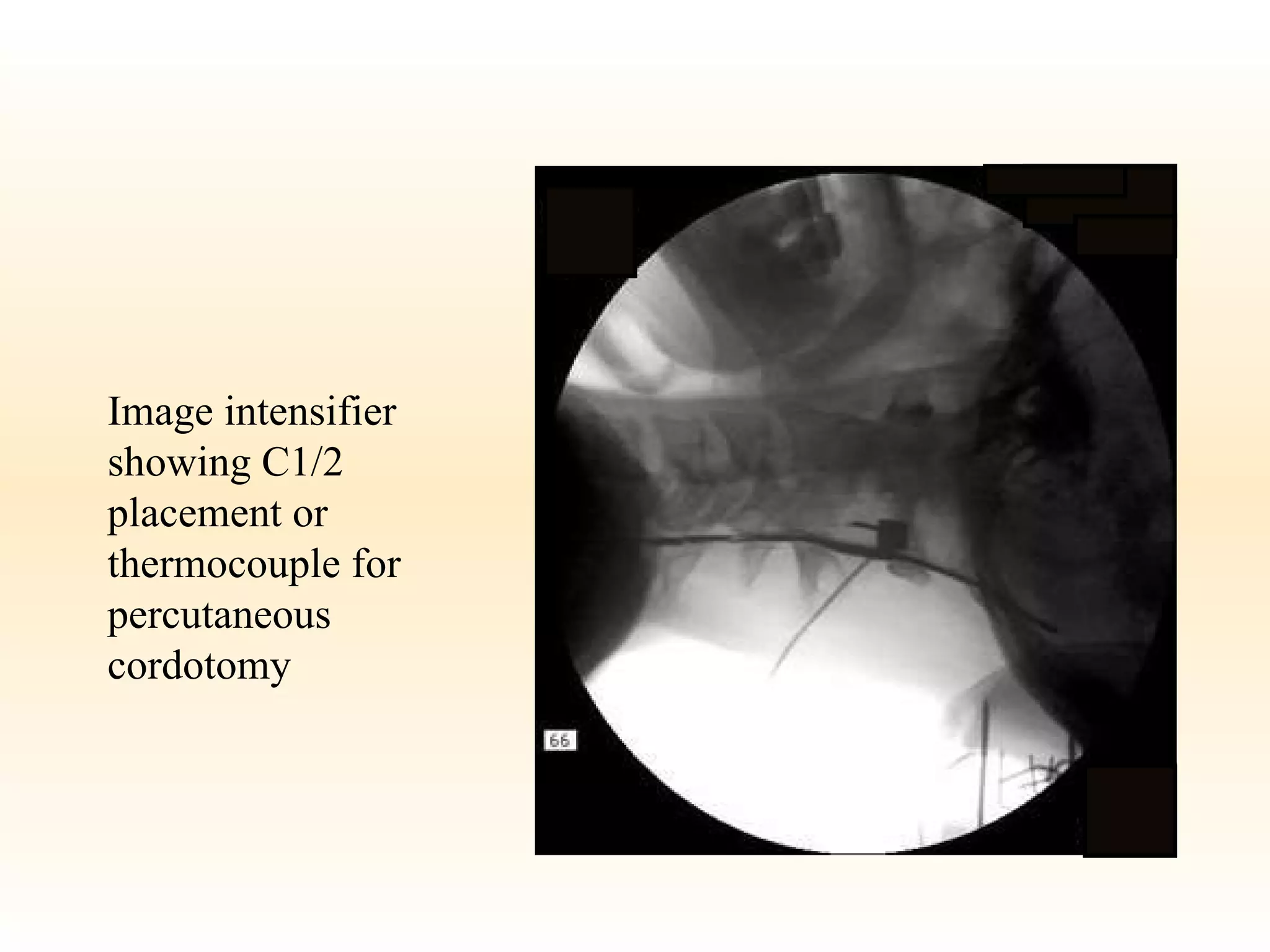
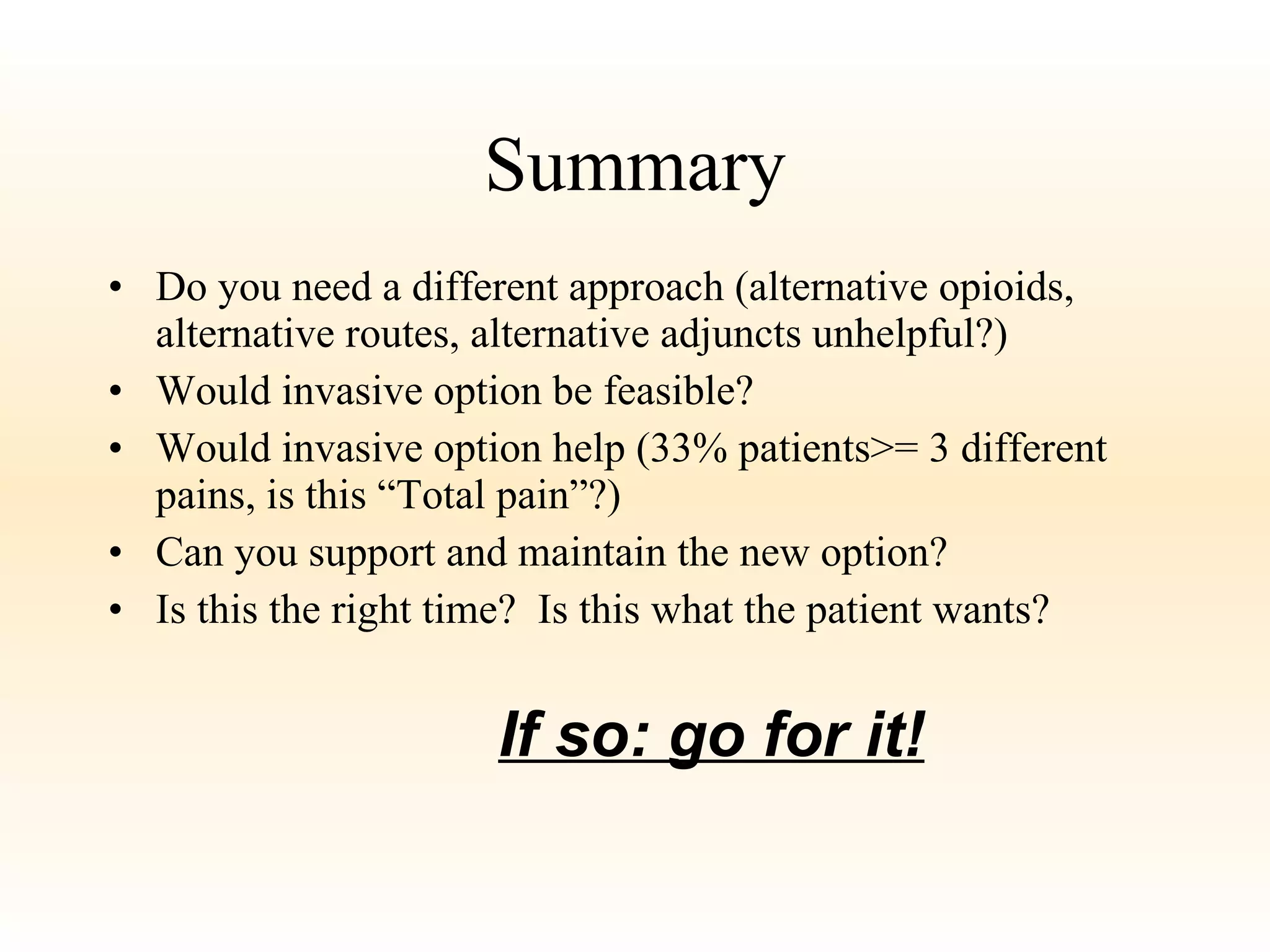
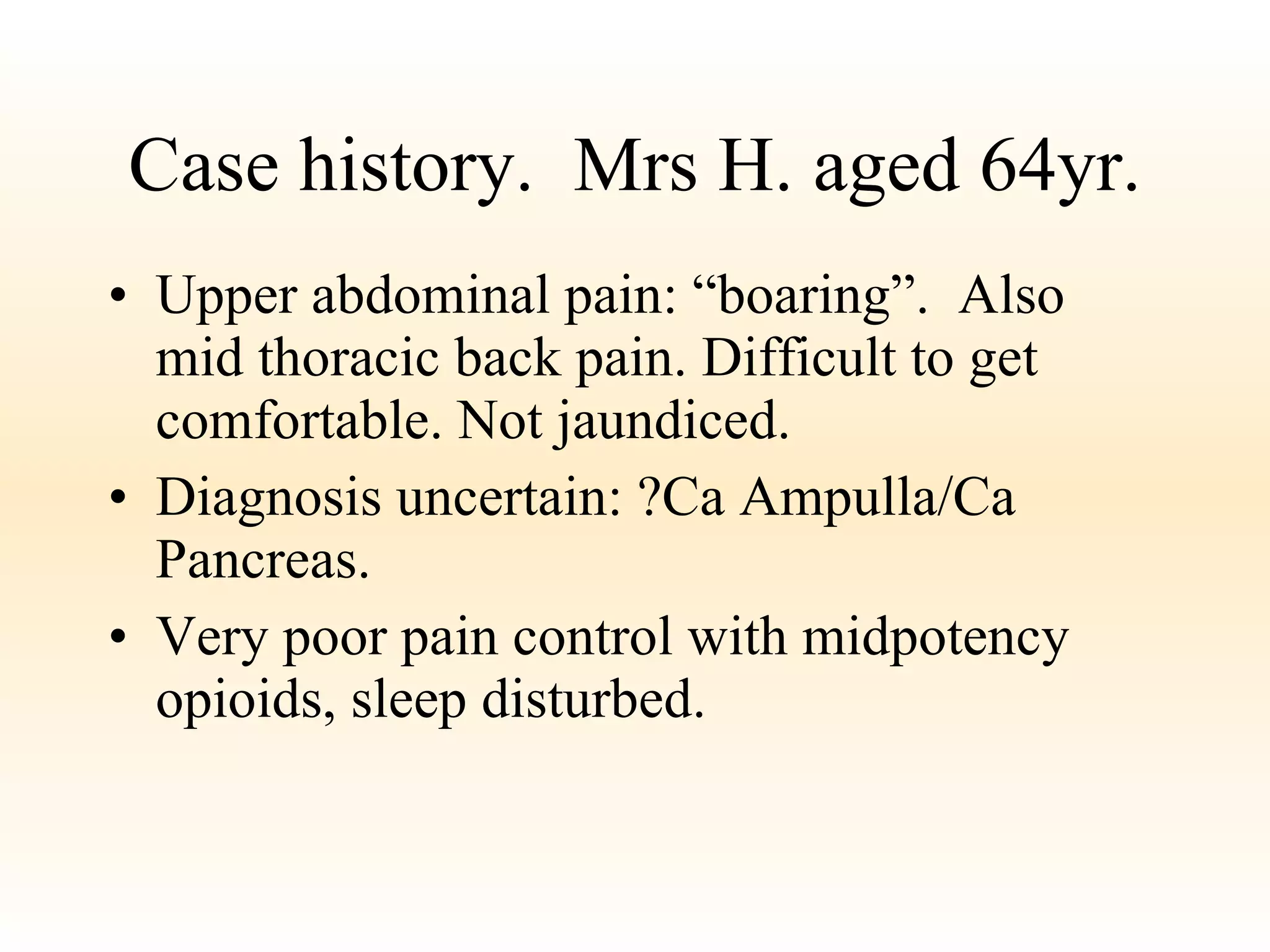
This document discusses various invasive pain management options for palliative care patients, including their indications, techniques, advantages, and disadvantages. It describes celiac plexus blocks, spinal/epidural infusions, intrathecal opioids, superior hypogastric plexus blocks, trigger point injections, and cordotomies. While some options can dramatically reduce pain, all have significant risks and limitations including side effects, technical difficulty, and potential loss of motor function. Invasive interventions are best considered when non-invasive options have failed to adequately control a patient's pain.