This document provides information on irritable bowel syndrome (IBS), including its definition, diagnostic criteria, subtypes, differential diagnosis, evaluation, and management approaches. Some key points:
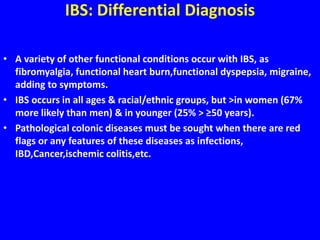
- IBS is a common functional gastrointestinal disorder characterized by abdominal pain and altered bowel habits. It affects 10-15% of the population.
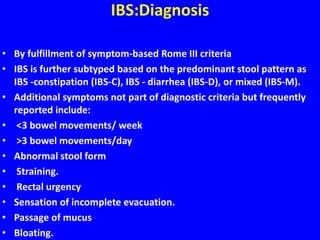
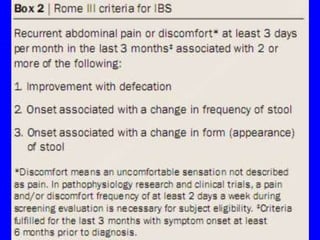
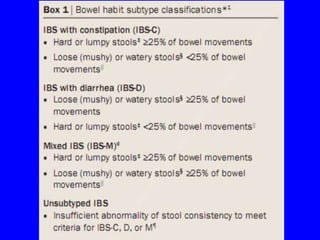
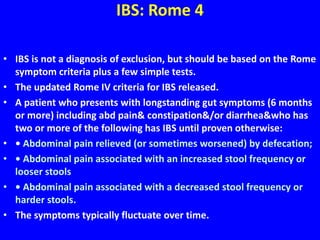
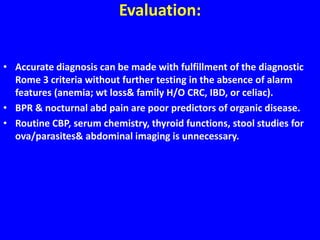
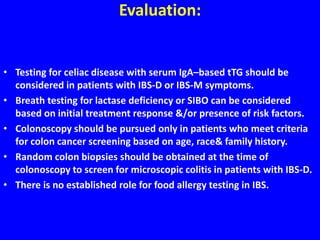
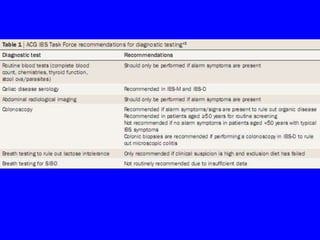
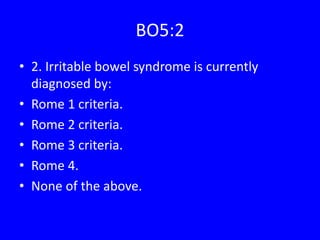
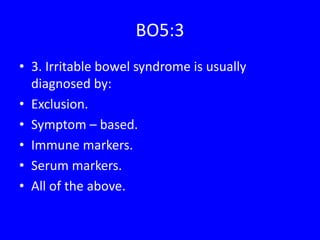
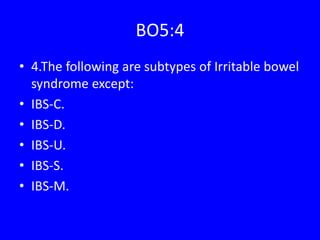
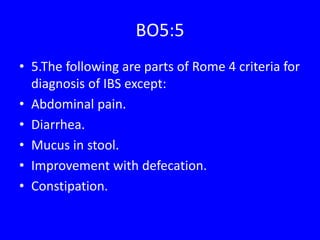
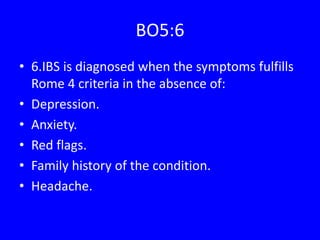
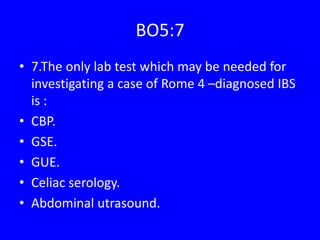
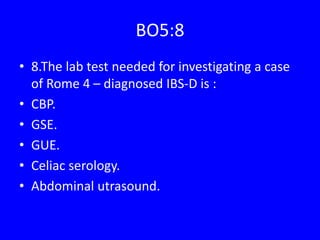
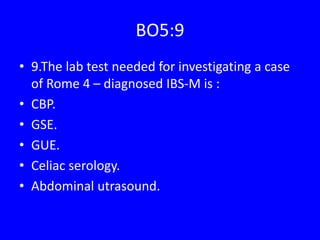
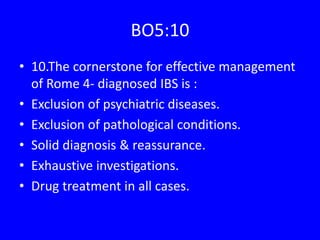
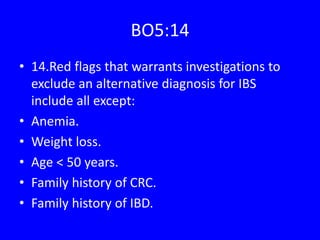
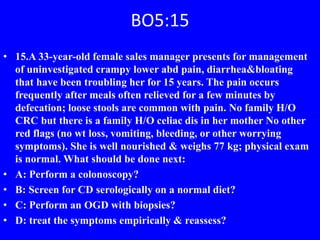
- Diagnosis is based on fulfilling the Rome symptom criteria, with subtyping based on predominant stool pattern. Additional testing is usually not needed in absence of alarm features.
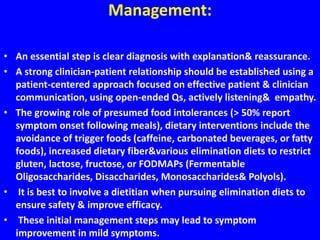
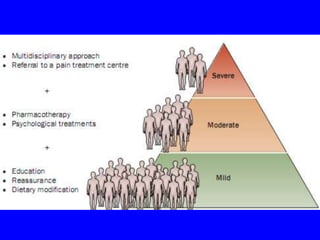
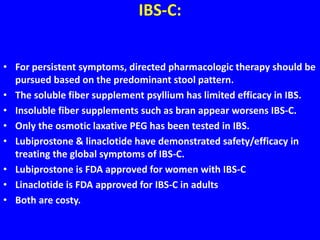
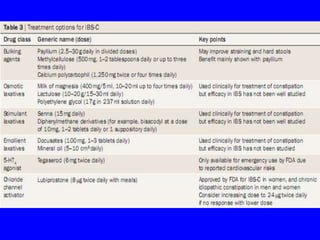
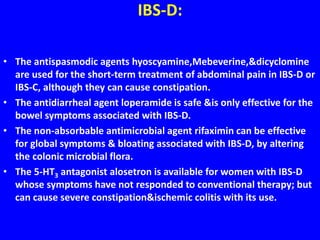
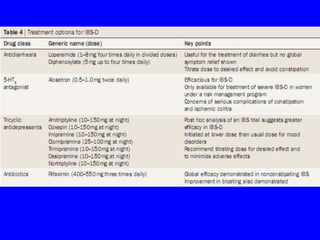
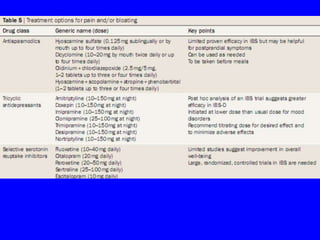
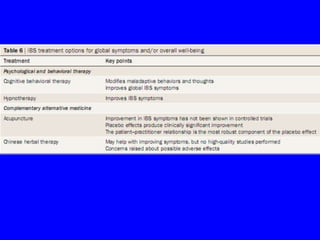
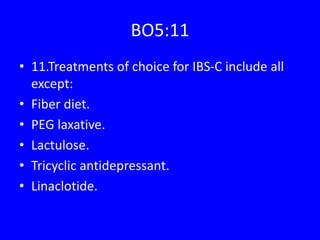
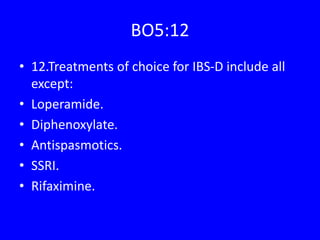
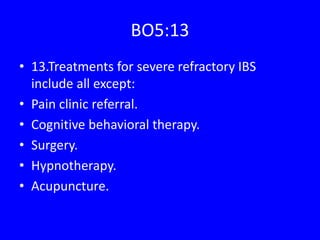
- Treatment involves reassurance, dietary modifications, antispasmodics, laxatives/antidiarrheals based on subtype, and tricyclic antidepressants/SSRIs for refractory cases.